Pimples under the nose: causes
The nasolabial triangle contains a large number of sebaceous glands and blood vessels. Therefore, rashes in this place are not uncommon. After all, the ducts of the sebaceous glands can become clogged for various reasons, and it is in this place that the skin is especially sensitive and reacts to any problems with the body. In addition, people often involuntarily touch the nasolabial triangle with dirty hands, provoking the growth of bacteria. So, for what reasons can a pimple appear under the nose?
- Due to hormonal changes in the body during adolescence or in women during menstruation, active production of sebum occurs. It clogs the pores and pimples form.
- A rash under the nose often occurs due to poor diet and liver or intestinal dysfunction. If toxins formed from too fatty and unhealthy foods are not eliminated naturally, they come out through the skin.
- Stressful situations, nervousness, lack of sleep provoke excess sebum production, which clogs the pores.
- Frequent runny nose and irritation of the skin under the nose leads to inflammation of the ducts of the sebaceous glands.
- Rashes also appear due to an allergic reaction to food, cosmetics or medications.
- Very often, black and white pimples under the nose occur due to improper facial care. Insufficient cleansing of the skin from dirt, particles of dead skin and the product of the sebaceous glands leads to the formation of a sebaceous plug.
Causes of sores
Most often, painful sensations appear after a runny nose - the mucous tissue is inflamed and damaged during cleansing of contaminants from the nostrils.
Microtrauma to the epithelium of the nasal passages can allow pathogenic microbes to penetrate deep into the cells, causing the delicate skin to become covered with a painful crust.
People who live or work in unfavorable environmental conditions (hot, dry climate, dusty, gassy rooms) can also suffer from dry nose and constant formation of erosions on the surface of the mucous membrane.
In an adult, the sore resembles a foreign object stuck in the nostril - the skin tightens and becomes covered with desquamated epithelium. As a result of removing the dry crust, bleeding and acute pain begin.
The reasons for this condition, in addition to a runny nose or sinusitis and constant stay in dry, dusty rooms, are different and not always harmless:
- Furunculosis - the beginning of the formation of painful suppuration begins with swelling of the skin, the area of the wings and the bridge of the nose. The skin turns red and feels hot to the touch.
- Sycosis is a disease in which pathogenic microbes (usually staphylococci) lead to inflammation of the hair follicles located at the entrance to the canal. In advanced forms of the disease, pus is constantly discharged from the nostrils.
- Allergies in chronic form - the pathology is manifested by constant itching and scratching, sneezing and lacrimation. As a result of constant irritation of the mucous membrane in the nostrils, signs of eczema appear.
- Erysipelas is a pathological condition that can affect the entire pharyngeal cavity, starting with the presence of multiple abrasions in the area of the wings of the nose. If wounds become infected, inflammation spreads deep into the tissue.
- Syphilis - the first sign of the disease is often a painful chancre. If left untreated, the lesion spreads to the bone tissue. Children can also suffer from the pathology (in its congenital form); in this case, the child’s runny nose does not go away and is practically impossible to treat.
- A tumor process is a painful ulcer that does not go away for a long time and may be a sign of the beginning of the growth of a benign or malignant neoplasm.
Before anointing a sore in the nose, it is better to determine what caused its appearance, because the body often signals the appearance of wounds and serious illnesses. Self-medication can eliminate the effect, but not the cause and will only do harm. Source: nasmorkam.net
Types of acne under the nose
Depending on the cause of its appearance and the characteristics of the body, rashes in the nasolabial triangle can be different. There are several types of acne, the treatment of which should be different.
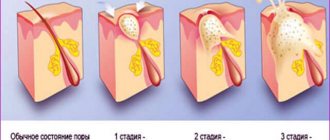
- Due to blockage of the ducts of the sebaceous glands, comedones are formed: black or white dots. This is sebum, skin particles, dirt accumulated in the pores. If the head of such a pimple comes into contact with air, it turns black. White pimples appear when the pores are closed.
- When an infection gets into such blocked ducts of the sebaceous glands, inflammation develops. A purulent pimple forms under the nose, which grows and, if not treated correctly, can spread the infection to surrounding tissues.
- Subcutaneous acne is very painful. They appear due to hypothermia or the development of bacteria. These pimples are usually red and inflamed.
Symptoms
Pimples on a child's nose can have a variety of manifestations. Depending on this, doctors make one diagnosis or another.
Prickly heat
The baby's sweat glands are not well developed. That is why the processes of thermoregulation in children proceed differently.
One of the most common factors in the appearance of a rash is prickly heat, which is quite difficult to distinguish on your own.
The situation is further complicated by the fact that there are several types of prickly heat:
- Red - in this case, the skin changes its shade. In the most difficult situations, it turns bright pink. Rashes with cloudy contents appear on the surface. Red skin color is associated with inflammation.
- Crystalline - many bubbles filled with clear liquid appear on the skin. They burst when pressed. This form of prickly heat is not accompanied by redness.
- Papular - it is characterized by the appearance of pinpoint rashes. They can form large patches on the skin.
- Infected is the most difficult option. In this case, microbes penetrate into the wound formed when the bubble ruptures. Bacterial microorganisms lead to the development of inflammation. There is also a risk of purulent complications.
How to properly treat acne
Most women try to disguise the rash or squeeze it out. But this often leads to the spread of inflammation. Therefore, if acne appears frequently, it is better to visit a doctor. After the examination, he will determine the cause of the rash. And only then can you understand how to get rid of acne under your nose. The most commonly recommended methods are:
- regularly cleanse the skin using special lotions;
- several times a day, treat problem areas with hydrogen peroxide and lubricate with medicinal ointments, preferably with an antibacterial effect;
- additionally use folk remedies;
- pay attention to your diet, change your cleansers;
- In case of severe rashes, avoid using decorative cosmetics.
What not to do to get rid of acne
Usually the rashes disappear over time without leaving a trace, causing only psychological discomfort to the owner. But if treated incorrectly, a pimple under the nose can lead to unpleasant consequences. To prevent this from happening, you need to know what not to do to get rid of acne.
- It is strictly forbidden to squeeze a pimple under your nose. In addition to the fact that this process may leave scars or ugly dark spots, it can easily become infected. There are many blood vessels in this place, so inflammation spreads quickly.
- Do not mask rashes with cosmetics. This can increase inflammation.
- It is not recommended to use scrubs during inflammation. They can injure the skin and lead to the spread of infection.
Traditional methods for treating acne
There are many recipes for cleansing facial skin. Some can dry out a pimple right away, while others are more suitable for preventing recurrent breakouts:
- For compresses and wiping the face, decoctions of chamomile, calendula, sage, yarrow, celandine and other herbs are used;
- you can treat rashes with aloe juice or tea tree oil;
- Orally, to cleanse the body, you can take birch sap, a decoction of birch leaves with honey, mint and thyme tea;
- a mask made from whipped egg white dries out acne and tightens pores;
- Steam baths with a decoction of calendula, sage, chamomile, mint, and burdock are good for acne.
There are crusts and sores in the nose, how to treat it, which doctor to see
When crusts or sores appear, the usual rhythm of life is disrupted. Unpleasant and quite painful sensations should be a reason to make an appointment with an ENT doctor.
At the appointment, the doctor will examine the nasal mucosa with a special instrument, only after which a decision will be made on the appropriate treatment.
Therapy for the presence of crusts consists of drugs of different release options (ointment, drops, spray).
Traditional medicine will also help in such a situation; it will remove sores from the nose without harm to health.
Modern drugs that are used to treat crusts in the nose include drugs from the following groups:
- Allergen blockers (Zodak, Diazolin, Cetrin).
- Medicines that increase the body's resistance to harmful influences (Eleutherococcus, Imunal, Apilak, Pantocrine).
- Antiviral (Acyclovir, Famciclovir, Penciclovir Valacyclovir).
- Stimulating immunity (Likopid, Cycloferon, Isoprinosine).
After visiting a doctor who has determined that crusts or sores in the area of the nasal mucosa are a staphylococcus infection, the following medications will be prescribed:
- Antibiotics;
- Antiseptics;
- Vasoconstrictor drops;
- Mucolytics;
- Nasal corticosteroids;
- Saline rinsing solutions;
- Inhalations with herbal decoctions;
What to do if a sore in the nose does not go away
A hard growth that forms a crust may appear singly or be a long-term “companion”.
Important! Usually such a sore goes away quickly, but there are cases when it is impossible to get rid of it for a long time. This may be a consequence of the fact that the wrong therapy is being carried out, which does not eliminate the original source.
For example, an ointment is applied to treat a fungus, but the sore is caused by a viral infection. The ointment should be used with caution by people allergic to such medications.
When a growth in the nose does not go away after a course of a certain drug, you will have to immediately consult a doctor.
He will determine the true cause of the sore in the sinuses. When such formations appear frequently, you should know how to prevent inflammation and dryness.
- During the season of illness, you will need to take medications to strengthen your immune system.
- With the onset of autumn and until the end of winter, it is necessary to drink a complex of vitamins and minerals.
- Use a saline solution to rinse your sinuses.
Three simple steps will help prevent sinus sores by strengthening the body's protective functions.
How to smear a sore under the nose - various remedies
Medicines that can be applied to a sore under the nose should be chosen taking into account the reason for which it appeared.
1. After mechanical impact of a foreign body on the nasal area, the resulting crust will need to be smeared with an antibiotic, which will have a local healing effect. If there is any foreign object in the baby’s nasal sinuses, you should immediately visit an otolaryngologist. He will remove it without risk to the child’s health. The most common drug for treating sores, in this case, is Syntomycin ointment.
2. Children get sick with colds and viruses at any time of the year. Sores under the nose that have formed due to a runny nose and inflamed mucous membrane can be effectively smeared with calendula ointment. This remedy will relieve the feeling of dryness and itching that arises from constant blowing of the nose and the use of drops to improve breathing. The bactericidal property of the drug will promote rapid healing of cracks and eliminate dry crust on the sore.
3. When the doctor has diagnosed an atrophic process in a child, as a result of which an ulcer appears under the nose, Actovegin or Methyluacil is used.
4. Herpes pimples that cover the area under the nose, doctors advise regularly treating the child with Auiclovir, applying Zovirax or Sulfur ointment. The active components of the drugs will eliminate pain and itching, which will be a great relief for the baby. In addition to pharmaceutical ointments, you can treat the sore with tea tree oil.
5. Sores that form a weeping effect on their surfaces must be shown to a pediatric dermatologist. Only by taking your child to an appointment can you receive the right recommendations for their treatment. After the examination and test results, the doctor will prescribe medications, including ointments: Erythromycin and Fukortsin.
Drug treatments
All medications can be used only after consulting a doctor. Most often, hormonal or antibacterial agents are prescribed. Antibiotics are first used externally, for example, Levomecithin, Tetracycline ointment or Levomekol. To normalize digestion and intestinal microflora, Bifidumbacterin, Laktovit, Filtrum Sti, and Hilak Forte are prescribed. “Polysorb” effectively cleanses the body, and it can be successfully used externally by treating the affected areas with a solution.
Doctors often recommend spot-applying Skinoren, Zinnerit, Baziron, Metrogil and others ointments on acne. A purulent pimple can be cauterized with iodine or Aspirin solution.
Nose ointment for infections
If the appearance of painful wounds is due to infection, what should you apply to the mucous membrane to speed up recovery and eliminate sores? A laboratory-confirmed bacterial infection should be treated with appropriate medications.
1
Tetracycline. Has antimicrobial properties. This is a broad-spectrum antibiotic, which in a concentration of 3% is used to treat runny nose, boils, viral eczema and other conditions that cause changes in the mucous membrane. The product can be applied three times a day to the tissue of the nasal passages, previously cleaned with an antiseptic solution.
2
Levomekol is based on antibacterial and restorative components, which many doctors recommend using in the treatment of infectious lesions.
If, after a severe runny nose or sinusitis, the mucous membrane is damaged and covered with painful ulcers, the drug is applied to gauze turundas and inserted into the nostrils. The duration of the procedure is half an hour, the frequency is three times a day. Before applying to wounds, the nasal passages should be rinsed with saline solution.
3
Another antibacterial drug in the form of nasal ointment is Bactroban. Contains the antibiotic mupirocin, which is active against staphylococcus, streptococcus and other infectious agents.
Use the drug for up to 5 days, applying it to the mucous membrane using an applicator. Then the nostrils need to be compressed for high-quality distribution of the product throughout the epithelium. A specialist will tell you which ointment is suitable in a particular case.
Black acne mask
To get rid of blackheads and small urticaria, many products are now on sale. Often women prefer natural herbal preparations. The best of them is now considered a black acne mask. A purchased product made in Brazil is more effective. This black mask is based on bamboo charcoal and also contains panthenol, propylene glycol, glycerin, grapefruit extract and wheat germ oil. It is applied to problem areas, and after half an hour is removed in the form of a film, drawing out all impurities from the pores. The same mask can be prepared at home: to do this, crush a couple of tablets of activated carbon and mix with whipped egg white. The film that cleanses pores is also made from gelatin.
How to quickly get rid of herpes under the nose
To remove herpes on the nose quickly, complex therapy is used. They drink antiviral drugs in tablets and at the same time apply them to the rash in the form of ointments. HSV does not spread to other areas. They use cauterization. The resulting crusts cannot be torn off; they are moistened.
To get rid of HSV on the face quickly, you can use Corvalol. It affects the sore spot without destroying the virus itself. Therefore, complex therapy is used to treat herpesvirus with this cardiac remedy.
Corvalol contains mint and alcohol, which dry out and heal blisters in the nasolabial triangle area. The drug eliminates the source of infection, preventing it from spreading to other places. If a person feels a painful tingling sensation, applying Corvalol will prevent the formation of bubbles. Advantages of the drug: low cost; can be purchased at all pharmacies; hypoallergenic; Possibility of use on the skin and mucous membranes.
At home, other methods are used to remove the rash. You can cauterize the affected area with a hot spoon and smear it with iodine. After cauterization, antiviral ointment is applied.
HSV is distributed throughout the world, and it is impossible to prevent its entry into the body. To prevent the virus from reactivating during an exacerbation, preventive procedures are carried out. It is necessary to wash your hands and face, strengthen the immunity of yourself and your children. If infected, do not contact other people. Use complex therapy. If treatment does not help, contact an immunologist and take an immunogram. This will help to find out which part of the protective system is broken. The immune system, having recovered, will cope with HSV.
source
Was the information helpful? Tell others about us, maybe they need help too.
Preventing rashes
After the pimples under your nose disappear, it is better to slightly change your lifestyle and diet so that they do not appear again. What is needed for this:
- eat less fried, spicy, smoked, sweets and fast food;
- avoid foods and cosmetics that may cause an allergic reaction;
- regularly cleanse your face of dirt using neutral products;
- walk in the fresh air more often and get a good night's sleep;
- stop smoking and drinking alcohol;
- additionally take vitamins A, E and B;
- once a week, do nourishing face masks or peeling to cleanse dead skin particles.
If you keep your body healthy and take proper care of your skin, then no pimple will appear under your nose.
The causes of a rash under the nose can be different. One of them is perioral dermatitis. This disease does not occur often, mainly in women. It manifests itself by the appearance of small reddish pimples on the skin of the face, in the area of the mouth and nose.
Other causes of such a rash can be: lack of skin care, allergic reactions, infection with the herpes virus, etc.
Treatment of fungal skin diseases
Any disease is easier to prevent than to treat. The same goes for skin rashes. To prevent a rash from appearing around a child’s mouth, it is important to follow basic hygiene rules:
- After each meal, the area around the mouth should be cleaned using regular washing with warm, clean water. If due to circumstances there is no water, you can get by with wet wipes.
- During periods of strong salivation (from three months and older), especially when teeth are being cut, the skin around the mouth is lubricated with zinc-containing cream. The zinc contained in the composition will prevent the skin from coming into contact with saliva, thereby preventing the occurrence of rashes.
- Dip the pacifier in boiling water before each use, as well as after a fall or prolonged sleep with it. High temperature can destroy all pathogenic bacteria that have managed to multiply on the surface of the product during sucking.
- Don't experiment with food. Pediatricians give explanations when introducing complementary foods: a child under three years of age should not be given potentially dangerous foods that can cause food allergies. Often parents want to please their child by treating him to bright and juicy orange juice. The result will be only red spots on the child’s body.
- In frosty weather, be sure to lubricate the child’s face with cream 15 minutes before going outside.
We suggest that you familiarize yourself with: From burns at home for a child
Important! The packaging of a cream that is applied to the face before a walk in the cold should not contain the inscription “moisturizing.” Otherwise, a cream with a moisturizing effect will only worsen chapping and cause frostbite.
Foods that have caused acne on the baby’s skin at least once should be discontinued, or the dose of consumption should be significantly reduced until the child is three years old. After reaching this age, you can again try to introduce such foods into the diet in small quantities, observing the body’s reaction.
Bathing a child
Daily water treatments and caring for your child's skin using regular baby cream will help keep his body healthy, protecting the baby from discomfort and itching.
As already noted, the rash can be primary or secondary. Primary rashes are of greatest interest because they are the most common. It is with their diagnosis that difficulties arise. Based on shape and appearance, the following varieties are distinguished:
- Tubercles are non-hollow lumps on the skin.
- Blisters are dense areas that rise above the level of healthy skin. Blisters are an allergic reaction to poison from plants and insects.
- Papules, or nodules, are non-hollow elements that differ in height and color from healthy skin. They usually go away on their own.
- Bubbles are small pimples. They have a pronounced center filled with cloudy liquid.
- Bubbles are large formations (from 0.5 cm).
- Pustules are pimples filled with pus.
- Spots are changes in the color of the skin.
- Roseola are small pink or red spots that disappear when you apply pressure to the affected area.
Roseola nursery
Red rash
Acne can also appear in a child due to poor hygiene. If the baby is covered with bright pimples, then this is a skin reaction to pollution, to which children are especially susceptible in the first 6 years of life. To prevent your child from becoming covered with a painful crust on delicate areas of the skin, carefully monitor the baby’s cleanliness and accustom him to water procedures.
A consequence of unfavorable thermal effects is hyperhidrosis, or prickly heat. It manifests itself most clearly in infants, starting at one month of age. The baby’s body has not learned to adapt to the ambient temperature, so spots appear on his head and shoulders from sweat. All treatment comes down to frequent exposure of the little patient to the fresh air and regular ventilation of the premises.
Red spots on the forehead, cheeks and shoulders are often a sign of allergies. During lactation, this means that the mother should adjust her diet and also abandon aggressive household chemicals.
Allergic rashes
Red pimples in a child are also observed with toxic erythema. The rash occurs in the facial area: on the head, forehead, cheeks, nose. Newborns and babies under one year of age are most susceptible to it. This type of rash does not require specific treatment and disappears on its own within 7-8 days. At a later age, erythema is rare and, as a rule, is a consequence of uncomfortable living conditions: humidity, ambient temperature.
Chicken pox rash
The most dangerous possible cause of skin changes is meningitis. The disease is severe and in some cases is fatal. A characteristic feature of the infection is a rapid increase in body temperature and the gradual spread of an itchy rash throughout the body. If you have the slightest suspicion of meningococcal infection, you should immediately consult a doctor.
White pimples
Milia, or white pimples, are a type of acne that occurs in adolescents during hormonal changes. They are a small cyst formed as a result of excess sebum. Appear on the cheeks, nose, forehead. The causes of milia are varied: poor diet, poor-quality cosmetics, hormonal imbalance. As a rule, rashes disappear on their own with age (at 15-16 years of age). If not, you should visit a dermatologist or endocrinologist.
The predominant localization of milia is the area around the eyes, cheekbones, and T-zone (forehead-nose-chin). It is impossible to squeeze out such a tubercle - the source is deep under the skin. To get rid of white pimples on the face, you need to adjust your diet and provide quality skin care by choosing products that correct the functioning of the sebaceous glands.
Similar rashes also occur in newborns and go away on their own within 1-2 months of life.
Milia in a newborn
Small colorless rashes that resemble nodules are called neonatal acne. Neonatal cephalic pustulosis appears on the face of children during the first month of life. This is how the baby’s skin reacts to the remnants of maternal hormones. No specific treatment is required - the baby will soon adapt to new living conditions. Acne usually goes away on its own within a few days, weeks or 1 year.
Colorless or flesh-colored watery pimples on the cheeks in later life may indicate a malfunction in the immune system: this is how a food allergy or reaction to emotional stress manifests itself. This phenomenon is called dyshidrosis. In emotionally stable children, it goes away on its own; otherwise, therapy is required, including the use of weak sedatives.
Rash under the nose: causes
The appearance of a rash under the nose may be associated with exposure to ultraviolet radiation on the skin, a decrease in the body's immune properties, increased sensitivity to allergens, the use of various creams and ointments, and high sensitivity of the facial skin to negative factors. In addition, there may be internal causes of the formation of a rash, such as pathologies of the digestive system, disruption of the normal functioning of the endocrine system, nervous strain and stress.
Rash under a child's nose
In children, the appearance of pimples in most cases indicates the presence of dermatitis. In such cases, you should contact your pediatrician and visit a dermatologist, especially if the child is less than three years old. You cannot give your baby any medications without a doctor’s prescription.
Non-pathological causes of a rash under the nose in children can be:
- dirt . Children often touch their faces with dirty hands and put various objects into their mouths. This may lead to rashes. If, apart from the rash, there are no symptoms of the disease, then you need to strengthen control over the baby’s hygiene, and lubricate problem areas with baby cream;
- weather conditions . Often, after a walk in windy or frosty weather, a child may develop small pimples or areas of damaged skin. You can cope with them with the help of baby cream, Bepanten, Summed and other similar products.
Rash under the nose in adults
Rashes under the nose, in the area of the nasolabial triangle, are often found in adults. The reason for this is the increased activity of the fat glands in this area. When bacteria enter the pores of the glands, an inflammatory process can begin, which leads to the formation of pimples, blackheads and rashes. However, the causes of a rash under the nose can be not only local; some serious diseases can provoke such a reaction.
The most common cause of acne and rashes near the nose is insufficient hygiene. If you are prone to developing a rash, you should use special products that reduce skin oiliness and have anti-inflammatory and antibacterial effects.
Of the common factors leading to rashes under the nose and on the skin of the face, hormonal imbalance is considered the most common. In women, pimples can occur during pregnancy or during menstruation. Pathologies of the cardiovascular and endocrine systems can also cause a similar reaction.
Treatment
If pimples are the result of a sexual crisis, then no treatment is required. The newborn is provided with routine care and hygiene procedures. In case of heat rash, it is necessary to ensure a normal temperature in the room and not to wrap the baby too tightly, devoting several hours a day to air baths. Local therapy involves the use of creams or powders (for example, Bepanten).
Diathesis during breastfeeding requires the exclusion from the mother's diet of foods with possible allergenic properties (eggs, red vegetables, citrus fruits, nuts, chocolate, seafood, etc.). If the child is fed an artificial formula, then it will have to be changed to another. They use drugs with antiallergic properties (sodium bromide, Suprastin, Fenistil), bathe the child in herbal infusions (chamomile, chamomile, oak bark).
Children's infections of a viral nature (measles, rubella, chickenpox) in most cases are treated nonspecifically. Antipyretics and antihistamines, interferon preparations and vitamins are prescribed. For chickenpox, the elements of the rash are smeared with antiseptics (diamond green), and measles requires eye washing and rinsing (in older children). But children with scarlet fever are prescribed antibiotics to which streptococcus is sensitive (penicillins, cephalosporins, macrolides).
A rash on a child’s face and nose cannot leave parents indifferent. It is necessary to find out why it arose and whether it poses any danger. But only a doctor will accurately determine the cause of the changes and tell you how to eliminate them.
Types of acne under the nose
There are several types of rashes under the nose. They differ in size, appearance, quantity and reasons for their appearance. Thus, small white pimples and blackheads usually occur due to lack of care. They are sebum or dirt particles trapped in the pores. White pimples are formed when a pore is clogged; subsequently they often become purulent and significantly increase in size, drawing surrounding tissues into the inflammatory process.
Small red rash under the nose
Various dermatitis appear as a small red rash on the face. They can occur as a result of an allergic reaction to ointments and creams, detergents or cosmetics used for treatment.
Rashes with dermatitis appear gradually, first the skin turns red, and then small nodules or pimples form on it. They may merge with each other, spread to other areas, but the lips and skin around them remain free of the rash. Itching and discomfort are often absent. Treatment of such rashes consists, first of all, in eliminating the cause of the allergy, and also includes a gentle diet and skin care.
Acne under the nose
Before acne appears, there is usually redness of the skin and the formation of several small pustules. Such rashes are accompanied by itching and pain. Acne under the nose can have several causes:
- Insufficient care.
- Hormonal disruptions and changes. Acne often develops in adolescents during adolescence, women expecting a child or who have recently given birth.
- Wrong diet.
- Allergies to medications, food or household chemicals.
- Stressful situations.
- Hot weather or increased physical activity, which is accompanied by profuse sweating.
- Internal problems of the body.
Pimples under the nose
Purulent pimples under the nose are often isolated, less often massive. The reasons for their appearance are similar to the reasons for the formation of acne. Often such rashes occur due to a lack of vitamins and minerals in the body, weakened immunity and internal diseases. The most common external causes are: improper skin care, poorly selected diet, exposure to adverse factors, etc.
Subcutaneous acne
Subcutaneous pimples are not as noticeable in appearance as purulent ones. They may appear as a bump of skin with no change in color, but may be reddish or pink. Such rashes are usually accompanied by severe pain. The reasons for their appearance can be various microorganisms, hypothermia, skin contamination and other factors. Subcutaneous pimples often become inflamed and purulent.
Clinical manifestations
Manifestations of the disease depend on the accumulation of HSV and the state of immunity. The following signs of herpes are distinguished:
- the appearance of characteristic bubbles with a clear liquid containing the virus under and inside the nose;
- low-grade fever (increase in temperature in the morning to 37.5 degrees, decrease in the evening);
- itching, redness, swelling of the skin around the rash;
- If left untreated, the blisters burst, forming erosions or ulcers.
Symptoms of the disease depend on the state of the immune system and the causes of herpes. The more a person suffers from colds, ARVI, flu, infections, the more often herpes is activated, causing the appearance of symptoms. With immunodeficiency, rashes form constantly and cannot be controlled.
Treatment of rash under the nose
Treatment of a rash under the nose includes, first of all, proper facial care. You should not squeeze out the pimples that have formed or try to hide them under a thick layer of cosmetics. Problem areas should be cleaned twice a day using special lotions; these areas should also be treated with hydrogen peroxide and ointments that have anti-inflammatory and antibacterial effects should be applied to them. It is better to avoid decorative cosmetics during treatment.
Among the folk remedies that help in such cases are compresses and rubbing with herbal decoctions (sage, yarrow, chamomile, calendula and others), treating the affected area with tea tree oil, aloe juice, birch decoction, and calendula tincture. You can also conduct a course of steam baths with mint, chamomile, burdock and other herbs.
A pimple on the surface of the skin occurs due to blockage of the sebaceous ducts. The secretions of the sebaceous glands cannot come out, they concentrate inside, form suppuration, cause inflammation and acne. Absolutely everyone has encountered this problem in their lives. In some cases, pimples under the nose appear unexpectedly and disappear on their own without additional effort. Why do they appear? What do they indicate? [ads-pc-1][ads-mob-1]
Nasal ointment for sores
How can you lubricate the skin inside the nose if a dry, painful sore suddenly appears or, conversely, a bleeding ulcer that causes a lot of discomfort? Propolis ointment is considered an effective and safe drug.
It has antimicrobial, anti-inflammatory, moisturizing and regenerating properties. The ointment increases local immunity, accelerates the healing of scratches and sores on the mucosal surface, and prevents their secondary infection.
1
Pinosol ointment is a product of natural origin based on eucalyptus and pine oils, vitamin E, thymol and menthol. It is used not only to quickly cure a runny nose and sinusitis, but also to get rid of their consequences in the form of painful lesions on the mucous membrane.
You can apply the product to the skin of the nostrils for atrophic, acute and chronic runny nose, when it is accompanied by the formation of ulcers and dry crusts.
2
Calendula ointment is no less effective in treating internal sores and wounds. It has a pronounced antiseptic and restorative effect, so dry crusts and erosions disappear quickly. To heal wounds, before applying to mucous tissue, doctors advise wiping it with a Chlorhexidine solution.
Causes of pimples under the nose
The nasolabial triangle contains a large number of sebaceous glands. The appearance of acne on the nose is provoked by external and internal factors. The causes of skin rashes are:
- active work of sex hormones;
- poor nutrition;
- stress, nervous tension;
- allergic rhinitis, colds;
- failure to comply with hygiene rules.
Cause of pimples under the nose #1 - hormones
Active hormonal levels cause increased activity of the sebaceous glands. The skin does not have time to cleanse itself in time, particles of dirt and dust join the secretions, and pores become clogged. Pimples appear under the nose. The situation is observed in absolutely everyone during adolescence, in women before menstruation, during pregnancy, after childbirth, during feeding, during menopause. It is very difficult to prevent the appearance of pimples under the nose in such cases. After all, it is unknown how hormones will behave. But while taking hormonal contraceptives, the situation can be easily corrected. Stop taking the pills or replace them with others. Hormonal imbalance is treated only under the supervision of specialists.
Getting rid of acne under the nose with folk remedies
People have a huge number of options for getting rid of skin rashes under the nose. They are also used for preventive purposes. Below are herbal decoctions and infusions that have proven to be the most effective.
- A decoction of burdock rhizome, St. John's wort, and celandine. All ingredients are taken in 1 tbsp. spoon. Pour in 500 ml of boiled water. Boil over low heat for 15 minutes. Leave for 1 hour. Use as a lotion 3 times a day.
- Tincture of elecampane, calendula, nut leaves. The preparation procedure is similar to 1 product. Dosage of ingredients – 1 tbsp. spoon.
- A product made from birch leaves, honey, birch sap. 1 tbsp. A spoonful of birch leaves is poured with 200 ml of water. Boil for 5 minutes. Cool. Add 100 ml of birch sap, 1 teaspoon of honey. Leave for 60 minutes. 2 tbsp. spoons are taken orally after meals. Treatment lasts 1 month.
You can quickly remove inflammation with aloe juice, tea tree oil, and an aspirin tablet. The remedy for acne under the nose is applied pointwise. Aspirin is ground into powder and a few drops of water are added. Leave for 20 minutes. The pimple disappears within a day.
Ointment for colds in the nose
Patients often ask ENT doctors to select a nasal ointment for a cold, being sure that the cause of the sores is the herpes virus.
Indeed, with this infection, itchy, painful rashes appear, but the symptoms are similar to bacterial ones, for example, staphylococcal.
You can make sure that it was herpes in the nose that provoked the painful rash only after taking a microflora test.
What ointment should I use to treat a viral infection? Doctors usually prescribe antiviral and immunomodulatory external agents:
1
Panavir is a gel with antiviral and local immunity-strengthening properties, has a herbal composition. You need to start applying the remedy for wounds in the nose as early as possible, using it 4-5 times a day for a course of 5 to 10 days in a row;
2
Tromantadine is an effective remedy against the herpes virus, which helps to avoid rashes on the mucous membrane if applied in time. At the stage of painful erosion after opening the ulcers, using Tromantadine is also effective - it relieves pain and prevents further inflammation;
3
Acyclovir - helps with sores left not only from herpes infection, but also from chickenpox. You can start using it from the first days so that the symptoms of itching and pain go away faster and continue until the crusts disappear;
4
Oxolinic is a drug that protects against viral infection when applied nasally. Used for the prevention and treatment of influenza, herpes, the product is safe for both adults and children.
You can anoint the inside of your nose against sores using a cotton swab with a medicinal product applied to it. Before use, you need to make sure that you are not intolerant to the components of the ointment. The standard course of treatment is up to ten days.