Symptoms and causes of keloid scar formation
Plastic surgeon Elena Viktorovna Salyamkina notes the following symptoms characteristic of a dissolving keloid scar:
- Pain.
- Increased sensitivity.
- Burning and itching.
- A scar raised above the skin level, with a hard and smooth surface.
- At the initial stage, redness is possible.
It is noteworthy that even after many years the scar does not lose its hardness and convexity. It has been noticed that most often such scars develop on open areas of the body, in particular on the earlobes, in the décolleté area, and on the neck. In some cases, scars occur on the joints, and very rarely on the face. However, with some probability, keloid scars can develop on any part of the body.
Some people may develop a keloid scar after mole removal. This is an unpleasant consequence that has reasons. Knowing them, you can avoid the formation of a defect.
Removing a mole is the right decision, since it can not only be an undesirable element on the skin, but also pose a danger in the form of oncology. But sometimes removing moles can lead to undesirable consequences, for example, the formation of a keloid scar.
When healing any damage to the skin, scar tissue forms - this is a normal process. But in some cases, this process can become pathological when scar tissue develops excessively. Excessive formation of scar tissue is called a keloid scar, or keloid.
It usually begins to form a few weeks after the mole is removed and can last for years. The formation of keloid scars is accompanied by characteristic symptoms. Among them, the most common are the following:
- soreness and sensitivity;
- itching and burning sensation;
- skin hyperemia.
A scar after mole removal can appear anywhere. But doctors point out that most often they appear on the earlobes, neck, and décolleté, that is, the most exposed areas. Keloids can also form on the face, but this happens very rarely. If a person has a predisposition to the formation of scars, then they can appear on any part of the body.
But why do keloid scars form? Doctors point to the following reasons:
- Improper skin care. It is not enough to simply remove a mole; it is important to follow all recommendations for skin care after surgery so that the postoperative period passes without problems and consequences.
- Predisposition. Doctors believe that the formation of keloids can also be hereditary. And in some people, the body is so prone to forming scars that they appear even after minor damage.
- Metabolic processes in the skin. For example, when collagen is produced excessively, scars can develop.
- Injuries. If the skin near the mole removal site is somehow injured, it can lead to scar formation. Even skin tension is enough, not to mention suppuration, infection, etc.
Knowing what factors can trigger the formation of a keloid, a person can avoid it.
Doctors divide the process of keloid formation into several stages:
- Epithelization. It is characterized by the formation of an epithelial film on the surface of the skin where the mole was removed. Over time, the film hardens, becomes rougher and becomes paler. The duration of this stage is from 2 to 2.5 weeks.
- Swelling. The keloid becomes even larger and rises above the skin level. The area where the mole is removed becomes painful and sensitive. The duration of the stage is from 3 to 4 weeks. After this period, the affected area becomes less painful, and the skin around the keloid becomes reddish and sometimes bluish.
- Seal. The keloid continues to change and lumpiness appears. It appears as a result of the appearance of local compactions, which over time fill the entire surface of the scar, but it still does not become smooth.
- Softening. Very rarely, the scar may become softer and more mobile. But this stage occurs extremely rarely; in the vast majority of cases, the keloid remains hard and rough.
The symptoms of a keloid scar can only be determined by a qualified surgeon. Do not self-medicate: if there is discomfort at the site of mole removal or your health condition worsens, consult a doctor. Symptoms of scar formation:
- pain that can be felt outside the place where the mole was;
- hypersensitivity;
- itching, painful burning;
- formation of smooth scar tissue;
- redness of the scar and the area around the site of inflammation.
Depending on the patient's health and the condition of the scar, symptoms may persist for several years. The external manifestations of the keloid also do not change: the scar remains elastic and hard. The most common places for keloid formation are:
- rib cage;
- neck;
- earlobes;
- joint areas.
Scar creams
You can improve the condition of the skin after removing moles with a laser or cauterization using medicinal ointments. Pharmacy products are used at home in the initial stages of scar formation. Absorbable and softening gels are most effective for shallow defects and are prescribed for complex treatment after laser resurfacing.
Creams for scars on the face and body:
- Contractubex has a softening, anti-inflammatory and smoothing effect on scar tissue, inhibits the growth of keloid feroblasts, relieves itching and irritation. The ointment helps remove atrophic and hypertrophic scars after mole removal. The gel is applied 2-3 times a day; for old scars, bandages are applied at night. Treatment is long-term and can take several months.
- Scarguard is a liquid cream made from hydrocortisone, silicone and vitamin E. The drug reduces inflammation, itching and swelling of tissues, and deeply moisturizes the skin. Tocopherol acts as an antioxidant, increases the elasticity of the epidermis, and stimulates cellular metabolic processes. The course of treatment is 1–6 months, the duration of therapy depends on how long ago the excision was performed.
- Kelo-coat is made from silicone. The drug prevents the formation and reduces the severity of scars, improves the aesthetic appearance of the dermis. After applying the gel, a protective film is formed that protects against the negative effects of external factors and liquid evaporation. The scars soften and gradually smooth out.
It is contraindicated to use pharmaceutical gels after removing nevi and moles without first consulting your doctor.
It is necessary to take into account the possibility of side effects, individual intolerance, the patient’s age, the presence of skin diseases, and inflammation. The combination of cosmetic procedures and the use of creams for external use allows you to achieve more effective results.
After removing moles from the body, there is a possibility that a bumpy scar will appear at the treatment site. The question of how to remove keloid scars worries many people - those who have already encountered this problem, and those who want to protect themselves from this after the destruction of the mole. The formation does not appear immediately, but by carefully monitoring the condition of the skin after surgery, the likelihood of avoiding such a negative consequence is reduced.
If you take the necessary measures to treat the wound, the scars after removing nevi will disappear from the skin.
Healing
A wound is formed at the site where the mole was removed immediately after the operation. Depending on the method of eliminating the defect, either a clear narrow scar or a spot appears on the skin. In most cases, a crust forms in the area where the skin was cut with a scalpel, damaged by laser, liquid nitrogen or electrical exposure.
This is a protective reaction of the body aimed at closing an area vulnerable to infection. In the first week - ten days, it is not recommended to carry out any physical impact on the area of the operation. Maintaining the integrity and tight fit of the crust to intact skin protects against infectious complications.
Scar creams
Special medicinal ointments and creams can help in the fight against scars. They increase the efficiency of procedures. The most commonly used include:
- Contractubex. The product softens the scar and has an anti-inflammatory and smoothing effect, relieves irritation and itching. It also slows down the proliferation of keloid fibroblasts. This ointment is applied to the scar three times a day. For old formations, it is recommended to apply compresses overnight.
- Kelo-cote. This drug has a silicone base. It has a softening and smoothing effect. Thanks to it, the growth of scars slows down, and the skin takes on a healthy appearance.
- Scarguard. This drug consists of hydrocortisone, silicone, vitamin E and tocopherol. The product is used to get rid of most of the unfavorable symptoms of skin diseases. It helps with itching and swelling, eliminates inflammation. Under the influence of the drug, cellular metabolic processes are activated.
How to Avoid Scars
To prevent the scar on the body from becoming inflamed after removal of a mole, prevention is required. All recommendations and prescriptions of the attending physician should be followed. Before the procedure, the specialist will determine the treatment strategy, check for contraindications, and prescribe the appropriate medicine for speedy healing of the scar.
After surgery, you must strictly follow the doctor's instructions, otherwise the spot will become inflamed, grow, itch, or fester.
To remove the seal, doctors prescribe liquid Contractubex. The recipe was developed by German specialists. The composition includes active components (onion extract, heparin and allantoin) that help achieve high efficiency in the treatment and prevention of scars.
Article approved
by the editors
Education can remain in the growth phase from 5 weeks to several years. In medicine, there are four stages of keloid formation:
- Epithelization. At the surgical site, a small inflammation forms, covered with an epithelial film. Over time, the film hardens and becomes denser. The color of the epithelium changes to light beige.
- Swelling. Occurs 2.5 weeks after surgery. There is a sharp jump in scar growth. An increase in size provokes pain, discomfort and increased sensitivity in the patient. A keloid can grow to unlimited sizes and exceed the boundaries of the previous mole. After 3-4 weeks, the sensitivity of the scar decreases, its size continues to increase or growth stops. The skin around the scar takes on a reddish or blue tint.
- Seal. Local compactions, the so-called “bumps,” form on the keloid. The deformation becomes more noticeable when the entire keloid scar is filled with bumps of different shapes and diameters.
- Softening. The scar loses its tuberosity and elasticity, becomes softer and more mobile. This stage is not typical for true keloids (this type is extremely rare). When a true keloid forms, irreversible processes occur that cause constant pain and inflammation of neighboring tissues.
Modern medicine still cannot indicate the true reasons for the formation of keloids. It is known for certain about the connection between postoperative care, the characteristics of the patient’s body and the mole itself. The main reasons for the formation of a keloid depend on the course and result of the operation. This is the main factor that has a direct impact on the condition of the scar. To minimize risks, it is recommended to carefully select the clinic and surgeon who will remove the mole.
Postoperative care is also important. The surgeon must explain to the patient how to treat and care for the wound that remains after the removal of the mole. The inflamed area is vulnerable and needs constant care. Most often, ointments, creams, and special sprays are used to heal wounds, as well as vitamins and mineral complexes to strengthen the body as a whole.
Keloid scars. Chief physician Nikolaeva-Fedorova Anzhelika Vladimirovna
Complications and consequences after mole removal: scars, scars, wounds, crusts and spots
Removal of keloid scars due to allergies to red pigment.
How to remove scars after surgery
There is an opinion that the formation of a keloid scar is influenced by genetic predisposition. The sensitive epithelium grows scar tissue even with the slightest scratch. When a scar forms, the excess tissue will be excessive, which provokes the formation of a keloid. The plasticity and speed of regeneration of the skin depends on collagen. With a high level of collagen, scar regeneration and restoration will be more successful in the shortest possible time.
Experts have not yet been able to fully determine the reasons for the formation of such scars. It is only known that they are associated both with the characteristics of caring for the wound after dividing a mole, and with the characteristics of the body of a particular patient. It is believed that this feature can be inherited. In addition, if a person is generally prone to the formation of scars, then he may encounter them even after a mosquito bite.
Presumably, the avalanche formation of scar tissue is influenced by increased collagen production in the skin. In addition, various suppurations, tension of the skin around the wound, and the like can also lead to the development of keloid.
After the wound heals, the epithelium is replaced by connective tissue, which is characterized by increased density and reduced functional properties. There are no hair follicles or sweat glands, and the cells are more susceptible to ultraviolet radiation.
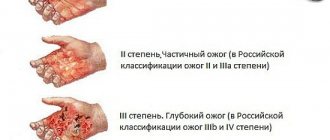
Scars after removal of large moles can be hypertrophic or atrophic. The first type is characterized by excessive growth of collagen fibers; a convex scar occupies a larger area than the size of the former nevus, rises above the surface of the surrounding skin, and looks like a rounded nodule. Atrophic scars, on the contrary, cause tightening of the dermis, and less connective tissue is formed than was previously healthy.
The process of keloid formation begins 2 weeks after epithelization of the wound and continues for several years. During this time, it enlarges, becomes coarser, and changes color from bluish, red to light pink. After 2–3 weeks, the new tissue swells, becomes convex, causes itching, and painful sensations appear on palpation.
After a month, the severe discomfort goes away, the skin around the scar turns red. The scar becomes dense to the touch and acquires an uneven, bumpy surface. After a long period of time, the keloid may become soft or remain hard forever.
Most often, scars form after removal of moles using classical surgery, cryo or chemical destruction. During the treatment, the skin becomes frostbitten or burns; further healing is accompanied by the appearance of scars.
Complications during the rehabilitation period can develop due to poor hygiene, non-compliance with doctor’s recommendations, the addition of a bacterial infection, inflammation, and suppuration. After regeneration of necrotic ulcers, the scars remain deeper and have jagged edges.
There is a genetic predisposition to the formation of a keloid; in such people, the prolongation of any injury is accompanied by a pathological proliferation of connective tissue.
The tendency to form scars is observed with increased production of collagen fibers in the skin.
After laser removal of a mole, scars remain in isolated cases. When exposed to a carbon dioxide ray, the liquid evaporates from the nevus and it is destroyed. There is no bleeding because the blood vessels are cauterized. During treatment, there is no direct skin contact with instruments or the doctor’s hands, this reduces the risk of postoperative infection.
Causes
Doctors have not yet developed a consensus on the reasons for the formation of keloids.
One of the reasons for the formation of keloid tumors is a violation of the integrity of the skin during surgery.
Epithelial tissue grows rapidly due to the excess collagen content in the body. Excess collagen leads to the appearance of a red keloid scar at the site of nevus removal.
On this topic
Experts consider the following factors to be important in the formation of keloids:
- Heredity is one of the main ways of development of many pathological changes in the body. The presence of keloid scars in parents increases the likelihood of the patient developing them after mole removal.
- Hormonal imbalances. The development of connective tissue under the influence of hormonal imbalance can lead to the formation of keloids.
- Careless and improper handling of the wound after mole removal. Under no circumstances can the protective crust be removed or picked out. Such actions are fraught with infection, pathological changes in epithelial tissues, and delayed healing of the wound.
- Damage fresh , healed wound, skin overstrain. This is facilitated by uncomfortable clothes (small, tight, rubbing, etc.), and excessive tanning.
- of collagen in the body leads to the growth of epidermal tissue in excessive volumes.
- Pregnancy period .
- Endocrine system , which works with disturbances.
The appearance of keloid scars is chronic in nature and requires periodic therapeutic courses of treatment.
Stages of neoplasm formation
After removal of a mole, a scar begins to form under the crust. After falling off, young pink skin is found in its place. At first, the scar is painful upon contact, then increased sensitivity, and over time, unusual sensations when touched disappear, and the elasticity of the tissue is restored.
The appearance of an uncomplicated scar also does not cause concern: the pink surface fades over time, the level of the scar is leveled with the general level of epithelial tissue, the skin looks healthy, and the site of damage is not noticeable. Complete healing of the wound surface occurs after removal of the mole in about a year. The scar at the site of surgical treatment or the area of non-invasive treatment is hardly noticeable by this time and practically does not stand out.
How to cure keloid scars at home - treatment with folk remedies
There are several basic ways to eliminate a colloidal scar after mole removal. Most modern people prefer to use medications. The most effective options include Lyoton, Hydrocortisone and Contractubex.
We suggest you familiarize yourself with Human papillomavirus in HIV infection
The first option includes the use of interferons. This is a good solution for those who have had moles and papillomas removed. Only a qualified doctor should prescribe and administer the drug. These methods include the use of corticosteroids and injections.
As for physical effects, the scar can be removed using laser resurfacing, surgery and electrophoresis. During surgical removal, the scar can be completely eliminated without causing any scars or other damage to the skin. If at this time germs or any objects get into the wound, a relapse may occur.
Another removal method is to expose the scar to x-rays. This option is only suitable if the defect was removed surgically. In such situations, relapse occurs quite rarely.
Traditional medicine recommends the following methods for removing keloid scars:
- compresses from infusions of chamomile, fennel, St. John's wort;
- massage with sea buckthorn oil;
- rubbing fresh honey;
- lubricating the surface of the keloid with rosemary and tea tree oil. These oils are essential oils, so they should be used in combination with a base oil;
- compress of crushed cabbage leaves and honey.
The effectiveness of these methods has not been proven. They can be used as an addition to the main therapy in consultation with the doctor.
Don't miss the most popular article in the section:
Hyaluronic acid tablets. Benefits, how to take, reviews from doctors and effectiveness.
Symptoms and causes of the appearance of a keloid scar after mole removal
After removing moles from the body, there is a possibility that a bumpy scar will appear at the treatment site. The question of how to remove keloid scars worries many people - those who have already encountered this problem, and those who want to protect themselves from this after the destruction of the mole. It appears formation does not occur immediately, but by carefully monitoring the condition of the skin after surgery, the likelihood of avoiding such a negative consequence is reduced.
Modern methods for removing moles and other skin formations make it possible to eliminate them quickly and painlessly. After most operations, there is not even a scar left that could remind of the operation. A keloid scar is a failure in the healing process of a wound that remains after the removal of a mole. It looks like a thickened and lumpy area of skin with a dark pink or bluish tint. The color of the formation depends on the age of the scar.
Such a scar does not form immediately after surgery, but over a long period. The healing process of the skin lasts up to a year, and a keloid scar will appear after 6 months (the timing depends on the size of the treated area of skin). In the first weeks, a new thin layer of epithelium forms on the skin. For a number of reasons, a failure in its growth is possible, due to which the new tissue grows and thickens, its color changes to a paler shade.
Reasons for appearance
Doctors have not yet been able to unambiguously determine the reasons for the appearance of such tumor-like formations. The factor of their appearance is damage to the skin during surgery. It is more likely that a keloid forms on the face, neck, back, and décolleté. Collagen is considered to be the culprit for the increased growth of the epithelium, or rather, its excess content in the body, which is why not a thin and inconspicuous scar appears at the site of the wound, but an unpleasant-looking red keloid scar. The main factors for the formation of a keloid include:
- hereditary predisposition;
- improper wound care;
- changes in hormonal levels;
- pregnancy;
- disruption of the glands of the endocrine system.
The keloid scar after removal of a mole is small, but, unfortunately, in most cases it is unattractive, especially if it is located in a visible place. Keloids themselves do not pose a danger to human health, and the main reason for their treatment is their unaesthetic appearance. In some cases, they may interfere with normal activities or rub against clothing.
A keloid scar forms at the site of a removed mole in about 1.5-2 weeks. During this time, the resulting layer of epithelium at the treatment site for some reason continues to grow and thicken. If you miss the moment and do not go to the hospital in the early stages to solve the problem, then In the future, this will lead to the growth and hardening of the keloid. The site of the removed mole requires careful care and proper treatment.
The main symptoms of colloid scar formation:
- redness of the skin at the site of removal;
- pain;
- itching and burning;
- slow but constant increase in size;
- lack of hair;
- location above the surface of the skin.
Many people may miss these important symptoms, arguing that if it itches, it means it’s healing. This approach is wrong and nothing but a rough keloid scar should be expected in the future. By postponing a visit to the doctor, the patient complicates further treatment. The older the scar, the it is more difficult to remove it and return the skin to a healthy appearance. But it is worth noting that even neglected and old keloids are not dangerous to humans.
A mole is a congenital or acquired pigmented skin formation. Some of them cause many problems, since they are located in the rubbed area, and with some you can live your whole life without noticing them at all. Moles are removed not only in order to eliminate the possibility of their degeneration, but also from aesthetic considerations.
A keloid scar consists of scar tissue that forms after the removal of a mole (scar tissue forms at the slightest damage to the skin, even scratches). If a failure occurs during the healing process, the amount of scar tissue becomes uncontrollable. A keloid is formed from excess scar epithelium.
At the initial stage, a keloid scar cannot be confused with another neoplasm. The shiny surface and rich red tint of the scar after removal of a mole indicates the need to consult a surgeon.
The formation of a keloid occurs several days or weeks after the removal of a mole, which depends on the size of the formation and the current condition of the patient. The keloid begins to grow, increase in size and harden. A keloid scar not only looks unaesthetic, but can also cause discomfort. At the beginning, it is quite noticeable, but begins to lighten over the years.
Home » Moles » Keloid scar photo after mole removal
A keloid scar is a pathological development of scar tissue. Wound healing after mole removal, as with other skin injuries, in any case leads to the formation of scar tissue. However, in rare cases, disruptions occur in this process: rapid formation of excess scar tissue occurs, which is why a keloid is formed.
The process of formation of a keloid scar usually begins a few weeks after surgery. And this process continues for a long time, up to several years. All this time, the scar continues to enlarge, grow and harden.
There are several stages of keloid scar formation. The first is called epithelization. At this stage, the damaged area is covered with a thin epithelial film, which over time begins to thicken and become rough. At the same time, its color becomes paler.
After 2-2.5 weeks, the next stage begins - swelling. As you might guess, at this stage the scar increases sharply in size. In addition, it is at this stage that pain after mole removal and increased sensitivity are observed. The scar already exceeds the size of the original lesion, and it protrudes above the general level of the skin. After 3-4 weeks, the pain decreases, the skin around the scar turns red, sometimes acquires a bluish tint.
Next comes the compaction stage. Local compactions appear on the scar and it becomes lumpy. Over time, it thickens along its entire length, but the tuberosity does not disappear.
In some cases, there is another stage - softening, when the scar becomes soft and mobile again. However, if we are talking about a true keloid, which, by the way, is extremely rare, the last stage does not occur. The scar remains rough and sometimes painful.
It is worth saying that if a keloid scar occurs, you should never self-medicate. It is imperative that you contact a good cosmetology clinic, where experienced specialists will examine the scar and choose the most suitable treatment method for your case.
By the way, there are quite a lot of these methods. The greatest results are achieved by their skillful combination. The most radical solution is surgery. However, this method is used extremely rarely, since there is a very high probability of a repeat scar at the site of the removed one. In this case, prevention of the development of a keloid scar is mandatory.
Let's consider the most popular treatment methods:
- One of the methods for smoothing scars is called electrocoagulation. The essence of the method is the effect of current on scar tissue, as a result of which it is smoothed and leveled.
- More than 220 years ago, it was noticed that local pressure on the scar area also helps to reduce it. For this purpose, special bandages with silicone inserts are used. The mechanism of action of this method is not fully understood. Today it is believed that pressure on the affected area causes atrophy of the vessels that feed the pathogenic tissue, as a result of which the scar decreases.
- An extremely popular method is cryodestruction, that is, the resolution of the scar under the influence of cold. However, this procedure is somewhat painful. In addition, very often a new, larger scar forms in place of the old scar.
- An alternative to this method was a combination of cryodestruction with microwave therapy. First, the scar is heated with microwave rays, and then the affected area is exposed to cold. This combination gives a much better and more sustainable result.
- Used for scar treatment and hormonal therapy. Hormonal drugs also give very stable results.
Listing all the methods for treating keloids is a difficult and time-consuming task. Yes, and there is no particular need for this. The choice of the most suitable procedure for you is made by a doctor who will explain to you all the features, pros and cons of a particular method.
It is necessary to carefully follow all the doctor’s recommendations for caring for the wound after removing a mole. Do not peel off the crust, soak it for a week, or expose it to ultraviolet rays. To do this, the affected area should be lubricated with sun protection cream, even in winter.
Any changes are a reason to be wary. For example, if the crust does not fall off for a long time, the wound becomes wet after removing a mole, or suppuration begins, you should definitely consult a doctor to prescribe further treatment. If you notice the first symptoms of the development of a keloid scar, it makes sense to start using the drug “Contractubex” after removing moles. It will slow down or completely prevent the development of the scar.
Good afternoon After removing a mole, a keloid scar began to form above my lip. I went to the doctor, they prescribed bukki therapy. Has anyone encountered the problem of keloids, how did you manage to solve it.
Scar removal methods
If, after removing a mole, a person notices that the skin healing process is pathological, it is better to consult a doctor. And the sooner this happens, the better.
There are many ways to eliminate a keloid scar.
Here they are:
- Electrocoagulation. Scar tissue is excised using current. As a result, the scar is smoothed out.
- Bandages. Using a special silicone bandage, pressure is applied to the scar, resulting in atrophy of the vessels that feed the scar tissue. As a result, the defect becomes smaller.
- Cryodestruction. The method involves exposing pathogenic tissue to cold. It helps get rid of the defect, but does not guarantee that a new, even larger scar will not form in its place over time. The cryodestruction procedure is also accompanied by painful sensations.
- Microwave therapy. This is an alternative to the previous method. First, the scar is heated with microwave rays, and then cryodestruction is carried out. The result is more lasting than from normal exposure to cold.
- Hormonal therapy. In this case, hormonal drugs are used, which gives a lasting effect.
- Surgical excision. This is a radical way to eliminate a keloid scar.
But you need to understand that the treatment and elimination of a keloid scar is the exclusive prerogative of the doctor. Therefore, it is better not to self-medicate, but to immediately contact a specialist.
Prevention of keloid formation
Scar formation is easier to prevent than to eliminate later. Therefore, doctors give their clients the following recommendations:
- Proper care. After removing a mole, a wound remains that needs to be taken care of. You cannot wet it for 7 days, and under no circumstances should you peel off the resulting crust. If the doctor prescribes wound treatment, you must strictly follow it.
- Protection of the damaged area. Until the wound has completely healed, it should be protected from the sun and cold. Your doctor may recommend applying sunscreen if the mole was removed on an exposed area of the body.
- Observe the healing process. Any changes should be noted. For example, if a crust does not form for a long time or does not fall off, the wound becomes wet, festers, etc., you should definitely see a surgeon.
Finally, to avoid any complications after mole removal, it is better to carry out the operation in the fall or winter. But the period of solar activity is not the best time for any manipulation of the skin in the surgeon’s office.
Complications
In rare cases, the restoration of the integumentary tissue does not go so smoothly.
If for some reason the wound does not heal by primary intention (multiple removal of the crust, repeated trauma to the surgical site), then the scar is not so flawless. The connective tissue spreads over a larger area, and there is a strong decrease in elasticity, which means limited mobility. But, sooner or later, in this case too, the functions will be restored, and healing will occur fully.
Keloid scar
An even rarer complication after mole removal is a keloid scar. This is a very unpleasant consequence that occurs for unknown reasons. It is believed that the following factors can provoke the appearance of excessive skin growths instead of the formation of a neat scar:
- deep damage to the epithelium;
- decrease in the body's immune forces;
- tendency to allergies;
- special conditions, for example, pregnancy, puberty.
But the most significant reason for the occurrence of a keloid scar is considered to be a genetic predisposition. In this case, a hypertrophied growth can occur even without visible tissue damage (in this case we are talking about a tumor of keloid origin) or at the site of the smallest scratch.
Treatment of postoperative scars
Uncomplicated healing processes after mole removal do not require special therapy. In some cases, a dermatologist may recommend emollient ointments and creams; in case of a large healing area, a course of physiotherapy is prescribed.
Keloid scar is a complex case. On the one hand, any physical impact can provoke rapid growth of connective tissue. On the other hand, in the absence of treatment, a significant cosmetic, physical and functional skin defect develops. Therefore, in each specific case, dermatologists resort to individual schemes for restoring skin smoothness. Doctors have the following tools in their arsenal:
- absorbable ointments (“Karipain”, “Kotnraktubex”, etc.) - daily rubbing, applying bandages;
- corticosteroids (“Triamcinolone acetonide”, etc.) – injection of a suspension of the drug into the growth approximately once a month;
- physiotherapy (electrical and phonophoresis with the flow of ions of absorbable agents into the tumor area);
- constant grinding of the skin surface - effective at the first signs of a keloid or after its surgical removal;
- excision of scar tissue with subsequent prevention of an increase in the amount of scar connective tissue;
- tight bandaging (bandage) with absorbable agents at the first signs of overgrowth.
The positive point in this situation is that keloids are not prone to degeneration into a malignant tumor.
Thus, the scar after mole removal in the vast majority of cases is neat and does not cause trouble to the person who underwent the operation. In rare cases of excessive scar growth, the dermatologist will select a treatment that is recommended to be strictly followed.
Mechanism of scar formation
Damage to the skin due to injury or surgery usually scars over time, leaving no marks on the body. But under unfavorable conditions, the regeneration process does not proceed correctly. Instead of ordinary cells, fibroblasts are formed in the damaged area. Their accumulations cause the formation of scars.
Connective tissue is denser and more susceptible to ultraviolet radiation. It lacks sweat glands. Keloid scars form from it. They come in two types:
- Hypertrophic. When they form, collagen fibers grow and form a raised scar. It has a larger area than the removed mole. This scar looks like a nodule rising above the surface of the skin.
- Atrophic. In this case, connective tissue is formed in less quantity than necessary. As a result, the dermis contracts, and a depression forms on the surface of the skin.
A keloid scar begins to form 2 weeks after the wound heals. The process may take several years. The skin changes color from red to pink, becomes rough and dense. Pain and itching may occur in this area. Then the discomfort goes away, and the skin around the scar becomes red, and the scar itself becomes lumpy and uneven. 3-5 years after the formation of the defect, a period of stabilization begins when no external changes are observed. Scars can increase under the influence of thermal or physical influences, or when they are damaged.