Possible causes of color change
Formation changes color only under the influence of certain reasons that you should be aware of:
- Changes in hormonal levels often cause color changes. It is observed in adolescence, in pregnant women, and during menopause.
- Excessive exposure. Occurs due to frequent visits to the solarium or prolonged exposure to the sun.
- For many, discoloration occurs after injury due to friction, squeezing, or tearing. Damage increases the risk of degeneration into a malignant nevus.
If a mole has turned black, it should not be ignored. Consultation with a dermatologist, oncologist, and passing the necessary tests will determine the nature of the changes. If necessary, treatment and removal of the nevus will be prescribed.
If the birthmark has lightened, there should be less concern, but ignoring the situation is unacceptable. An alarm should appear if there were no visible reasons for the color change.
Experts have identified a number of accompanying factors leading to the degeneration of a benign tumor into melanoma. The risk increases when:
- skin, light hair. This way you can get a sunburn on your face and back faster;
- there is a hereditary factor;
- there are convex hanging moles, soft formations with a blurred contour, protruding above the surface of the skin;
- a person has a large number of nevi (more than 50);
- constant exposure to the open sun, artificial tanning;
- nevi are located in places subject to constant trauma, pressure, and friction;
- Inflammatory processes develop on the skin where the spots are located.
Possible causes of a blackened mole
Blackening of a mole may not always be a signal of cancer. First of all, the following factors can influence the change in their color:
- Hormonal disruptions and changes in the body, this can be female menopause, pregnancy, adolescence, thyroid disease.
- Mechanical injuries of both flat and hanging nevi.
- Exposure to ultraviolet radiation, with prolonged exposure to the sun or in a solarium, can provoke an increase in the amount of melanin, as a result, black spots may appear on the mole.
Those who naturally have a lot of birthmarks, and even more so if they are dark, need to carefully protect them from the sun, because they can become even darker. To prevent such growths on the body from changing color, you need to follow several rules for staying in the sun:
- Sunbathe only in the morning and evening, when the sun is not so harmful and active.
- Do not cover moles with adhesive tape, especially in the summer; doctors are categorically against this, since a greenhouse effect is created, this can cause darkening and even infection in the body, because with a lack of oxygen, small ulcers appear.
- Don't get carried away with the solarium.
- Rest according to your skin type, for example, for fair-skinned people with numerous birthmarks, it is better to replace the sea coast with a more wooded area.
If pigment spots turn black with age and this process is almost invisible, then you don’t have to worry too much. But suddenly, in a fairly short period of time, the nevus became black, and also changed its shape and size, this may indicate its degeneration and you should urgently consult a doctor.
Presence of accompanying symptoms
Changes in the color and structure of a mole are signals that processes are running inside the body that you should be aware of. Does not always indicate the presence of a tumor. You should keep the condition of the pigment spot under control by regularly undergoing examinations by an oncologist and dermatologist. Experts will identify the true cause of this condition.
The following symptoms may indirectly indicate malignancy:
- the shade of the spot became a rich dark black color;
- the hanging nevus fell off;
- change in size and shape: drying out or rapid growth;
- the appearance of itching, pain. The spot itches periodically or constantly, becomes dry, and microcracks may appear;
- the appearance of bumps and irregularities on the surface of a previously flat mole;
- redness along with changes in boundaries. They become asymmetrical and gradually blur;
- the appearance of a bloody, white discharge even without affecting the area.
If one of the alarming signs appears, you should visit a doctor, he will give you a referral for the necessary tests. The combination of symptoms indicates the need for urgent examination.
Is this dangerous and should you see a doctor?
If a mole changes color and shape, urgent consultation with a specialist is required. Ignoring the situation often leads to the degeneration of the formation into melanoma. It is worth considering that with age there is a natural change in the shade of birthmarks. It happens unnoticed by a person, gradually, and does not pose a danger.
Separately, we should consider the situation when a brown nevus suddenly turns red, acquires a blue, wine tint, and pain, itching or burning appears. A doctor can determine the exact cause of the condition. Self-medication is strictly prohibited. After the examination, the doctor prescribes a histological examination. If the answer is positive, the person should additionally undergo an MRI, CT, or ultrasound.
Based on the results of the examination, the type of tumor, stage, and the presence or absence of metastases affecting other organs are determined. A malignant formation requires surgical removal. Chemotherapy and radiation are indicated for those who have metastases.
In individual cases, mole removal is recommended. One of the methods is used:
- Surgical.
- Laser.
- Radio wave.
- Cryodestruction.
- Electrocoagulation.
Dermatologists and oncologists recommend removing nevi located in places of constant injury or rubbing. If the cause of redness is sun rays, a visit to a solarium, or other external factors, removal of a mole is not a mandatory procedure.
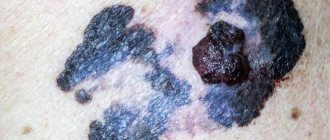
What dangerous moles look like
Why do people with nevi on their bodies need to monitor their changes? There is always a threat of degeneration of non-dangerous tumors into a cancerous tumor. What moles are dangerous to health? Key signs you need to know:
- change in shades towards the dark side, the appearance of multi-color;
- rapid increase in size - exceeds two millimeters per year;
- occurrence of cracks;
- the formation of asymmetry due to uneven growth;
- lack of elasticity;
- the appearance of itching, burning;
- presence of discomfort.
The appearance of dangerous moles requires an immediate visit to a specialist to clarify the nature of the changes and the likelihood of developing skin cancer. Pathological transformations provoke:
- injury to the nevus due to negligence;
- self-removal;
- abuse of exposure to the sun, use of a solarium;
- location of the formation in places of frequent contact with clothing - on the neck, head, genitals, legs;
- placement in the hair, on the face, palms - where there is a high probability of injury;
- previously removed melanoma.
Not a single person is protected from the sudden proliferation of cells of a harmless mole. Melanoma is an extremely serious disease. Changes not detected at the initial stage can result in death. The provoking factor is unsuccessful independent removal of tumors. Moles are dangerous because of their ability to:
- transform into an atypical – precancerous form;
- grow to large sizes;
- turn into cancerous;
- with minor external changes, metastases actively spread throughout the body through the circulatory and lymphatic channels.
What do nevi that are subject to pathological changes look like? Only a doctor can correctly distinguish between non-dangerous tumors. Dangerous formations look like this:
- blue – seals under the skin with clear boundaries, with dimensions no more than 10 mm;
- nodal – round, flat in shape, color – brown, black;
- skin – often pale, convex;
- halo nevus - pigment surrounded by a light or white rim;
- Spitz - looks like a dome-shaped tumor of pink shades, with the possible presence of a hole through which blood and fluid leaks;
- connective - connect individual formations into a whole.
One of the signs of a non-hazardous formation turning into a dangerous one is a change in contours. It often has blurred edges and scalloped borders. There are non-dangerous types of nevi - dysplastic. Only a specialist can make a correct diagnosis. A mole with uneven edges can be dangerous if there are additional signs of melanoma:
- accelerated changes in size;
- the presence of clearly defined asymmetry;
- the appearance of highly indented boundaries.
Prevention of malignancy
A person cannot completely protect himself from the possibility of a mole degenerating into a malignant formation, but following a number of recommendations can to some extent reduce the existing risk.
- Sunbathing is prohibited from 11:00 to 17:00 – a period of strong solar activity.
- Frequent visits to the solarium can negatively affect your health. The procedure should not be too frequent or lengthy.
- The skin should not be constantly in contact with chemicals.
- It is recommended to exclude from the diet foods with food dyes and chemical additives that increase the risk of developing cancer.
- It is forbidden to comb, rip off, or remove nevi yourself.
- The appearance of symptoms of degeneration should be a reason to visit a doctor and undergo the necessary examination.
Many people do not pay attention if a mole becomes burgundy, becomes lighter, or turns pink when it was dark. Ignoring the situation that has arisen does not always have a detrimental effect on health, but it can also be a symptom of malignant nevus. A timely visit to a specialist will help to identify the true cause of the situation and correct it in a short time without harm to health.
Causes of painful nevi
As you grow older, moles on your body only grow. But what is the reason for this process?
The most common factors that influence the increase in the number of moles are:
- Injury to the surface of the nevus. Impacts, injections, and incisions in the epidermis at the location of the nevus are not uncommon, but one of the most pressing issues is the situation in which the patient tore off a mole. We will consider what to do in this case below, however, mechanical damage to the pigmented tissue of the nevus is one of the leading etiotropic factors causing pain.
- Burn of any nature. Thermal shock can cause intense pain in the epidermis, which is especially pronounced in areas where moles and age spots are located.
- Hyper- or hypothermia. Increased or decreased body temperature may be accompanied by a feeling of soreness in the skin, especially in places where moles are located.
- Malignant transformation. Evidence of the onset of the oncological process may be pain, which is associated with the fact that the mole is inflamed. What to do in this situation can only be suggested by a specialist in the field of oncodermatology, who will not only perform a visual examination of the inflamed area of the epidermis, but will also prescribe a series of diagnostic measures to identify the prerequisites for the development of melanoma. After receiving the research results, the doctor will determine the most rational concept of therapy or recommend removing the inflamed nevus.
The last factor is by far the most dangerous, as it is associated with uncontrolled division of skin cells, which leads to cancer.
As mentioned above, a sign of oncological degeneration can be an inflammatory reaction, which, in addition to pain, is also manifested by swelling, redness and itching of the location of the mole.
This is due to mechanical trauma to surrounding cells during tissue proliferation. Often this process is accompanied by an increase in the size of the pigmented formation.
It is also important to note that sometimes during malignant transformation, a small white spot (halo) may form around the body of the mole, which is caused by a reflex vasospasm.
The most common reasons for the degeneration of a mole into a malignant formation include excessive doses of ultraviolet radiation and mechanical damage.
Those who believe that white-skinned people are more susceptible to melanoma are deeply mistaken. Melanoma can affect anyone, regardless of their skin type.
A sharp increase in the number of birthmarks, excessive growth, changes in the color of the skin around, namely redness, discoloration and any disturbance in the color of the birthmark, itching, peeling, tingling sensation inside should be a reason for an immediate visit to a specialist.
A nevus can darken as a result of:
- hormonal changes, for example, adolescence, the onset of menopause, the use of hormone-containing drugs, thyroid disease;
- mechanical injuries of neoplasms (cuts, burns, etc.);
- exposure to UV rays (solariums, prolonged exposure to the open sun contribute to the body’s production of melanin, which affects skin color).
A color change can be observed both on the entire surface of the formation, and only on part of it.
Changing the color of hanging moles
The cause of darkening of a mole on a leg is most often a mechanical injury. Such a neoplasm protrudes above the surface of the body, and constant friction of the nevus on clothing and squeezing can cause it to turn black.
In addition to mechanical effects, darkening may be associated with changes at the hormonal level and under the influence of UV rays, which are dangerous for such formations.
READ MORE: When can you wash after mole removal?
Change in skin color around the circumference
A changing shade around the tumor may be a signal of concern. What diseases are indicated by color changes in the halo:
- A brown field is characteristic of seborrheic keratosis. The disease is hereditary and appears after sunbathing.
- Dubreuil's melanosis is a malignant neoplasm in which the brown color around the mole is of unclear shape and with different shades.
The most dangerous phenomenon is redness and blackening of the skin around the mole. The skin can turn red as a result of injury, as well as when the sebaceous glands are clogged. A black tint most often indicates melanoma.
The darkening of a mole to black is caused by the following factors:
- Ultraviolet. Exposure to direct sunlight causes an increase in melanin levels. Moles that are constantly exposed to ultraviolet radiation change color to a darker color;
- Hormonal changes. The restructuring that occurs in the body during adolescence, during pregnancy, during menopause, and endocrine disorders can contribute to a significant darkening of moles;
- Damage. Mechanical impact on the mole during shaving, scratching, washing with a hard washcloth, and even simple friction with tight clothing can damage the formation, which will begin to darken due to subcutaneous hemorrhages.
Note! If the mole is not completely blackened, but partially, this may indicate its degeneration. You should immediately consult a doctor, preferably an oncologist.
Why did the mole change color?
If a mole has changed color, this should alert you. Nevi are skin cells with a high concentration of pigment. It is not at all necessary that it will be a brown pigment; black, red, and even blue moles are often found. This is the difficulty of determining which of them are dangerous and which are not. This often depends on genetic predisposition, as well as the frequency of skin exposure to ultraviolet radiation. Doctors have proven that red moles are the safest, since the nature of their origin is different - they are vascular pigment spots that occur when the subcutaneous capillary network is damaged. Accordingly, it is dark nevi that are considered the most dangerous, because they are prone to degeneration into malignant neoplasms.
What should you pay attention to?
It is difficult to find out which of the many moles on the body can develop into malignant melanoma. That is why you should regularly visit a dermatologist, especially for those who have “problematic” nevi on their body, located in places of constant contact with clothing.
Due to regular mechanical impact, even normal moles can be damaged, which gives the first impetus to their degeneration. Attempts to remove moles on your own using alternative medicine recipes are strictly prohibited.
Improper exposure to a nevus can worsen its condition and accelerate the process of its degeneration into melanoma. Unscrupulous employees of beauty salons, when performing the procedure, can introduce an infection into an open wound, which also causes many problems and requires long-term treatment. It is better to consult a doctor and choose the optimal removal method in a reliable clinic under the guidance of a qualified specialist.
In order not to miss the moment when a mole has changed color, it is important to regularly examine the body, because not only the color, but also the shape can change - from flat to convex or uneven.
What are moles: types and photos
There are many varieties of such formations. They are:
- light and dark in color;
- protruding above the surface of the skin and flat;
- deeply embedded in the thickness of the skin and superficial.
Often small moles give a special zest to its owner, but there are times when large formations on the face simply disfigure a person’s appearance.
All types of nevi are conventionally divided into 2 types:
- vascular, which include papillomatous formations and angiomas;
- pigmented, among which are freckles and lentigo (a uniformly pigmented flat spot of brown or black color).
In addition to melanoma, there are other types of skin cancer (squamous cell skin cancer, basal cell carcinoma), however, unlike melanoma, they are much less aggressive and are more treatable.
Basal cell carcinoma or squamous cell carcinoma of the skin appears as a long-term non-healing crack or wound, which is usually located on the face, neck, or back of the hand.
- Lentigo - this pathology can only be observed in elderly people. Melanoma is localized in the face and neck. It protrudes slightly above the skin.
- Knotty. Refers to aggressive forms of oncology. Visually it looks like a cluster of nodules of different sizes and colors. The tumor may grow high above the skin and be black or purple in color.
- Superficial melanoma is the most insidious type of cancer. Due to the fact that the tumor does not protrude above the skin, it is difficult to distinguish melanoma from a mole.
- Subungual melanoma is located under the big toe nail. It is found in every 10 melanoma patients.
READ MORE: What is the name of a mole doctor?
Important! One of the first signs of degeneration of a mole is the “ugly duckling” principle or its difference from other nevi on the body.
Any mole on the body, under the influence of certain factors and causes, can degenerate into a malignant tumor, dangerous to health and life in general. There are the following types of moles:
- Borderline. These moles are dark spots of regular shape and uniform color; they do not react to ultraviolet radiation, do not grow larger over time and do not change color.
- Flat. Usually these are light or dark pigmented formations of a flat shape, located in the upper layers of the epidermis. The number and size of such moles changes throughout life.
- Convex. Such moles form in the deep epidermal layers, are characterized by a convexity, as well as a smooth or bumpy structure, sometimes hair grows on them.
- Epidermal-dermal or birthmarks. They are usually large and flat, but can rise above the skin.
- Complex. These moles appear throughout life, they protrude and hang, are represented by irregular shapes and complex colors.
- Hereditary. These formations on the face or body are present from birth and are characterized by irregular shape, convexity and complex colors. Usually these are large moles - up to 12 mm, their boundaries are not clear.
- Blue. These moles are bluish in color, without hair, smooth and convex.
- Reds. These are benign moles of vascular origin.
- Senile keratomas. These tumors usually appear in old age, their density and size can vary, and their color varies from pink and brown to black.
Almost every person has moles. Some people have only a few of them, while some people can count dozens or even hundreds of such marks. Most moles are harmless. But among them there are specks that can cause a lot of trouble. What types of moles are distinguished and when do they require our close attention?
Morphological classification of moles
A mole in medical terminology is called a “nevus”. This is a cluster of cells - melanocytes, containing a special pigment - melanin. The color of the mole is determined by the concentration, quantity and depth of melanin in the nevus.
Moles are classified according to a number of parameters. They may vary in color, shape and size.
The color range of spots is varied. It depends not only on the characteristics of the cells that form the mole, but also on the color type of the carrier’s skin. Available palette:
- From light brown to almost black.
- Pink - red - crimson.
- Blue - purple - dirty blue.
Flat and convex, round and oblong, nodular and “pedunculated”, smooth and rough - the dimorphism of spots is impressive! As a rule, even on the body of one person, moles of various shapes can “get along” quite peacefully.
Size
From 1 mm to extensive nevi covering a significant area. As a rule, size is not directly related to the risk of nevus degeneration into an oncogenic form.
Attention! Any change in the shape, color, size and structure of the nevus is a sufficient reason to contact a dermato-oncologist for timely diagnosis!
Moles that have:
- smooth edges;
- no more than 0.5 cm in diameter;
- evenly colored.
Even the subjective feeling that a mole is different from the rest, and even more so that it is itchy, growing and changing color, should alert you. According to some data, the 5-year survival rate after treatment of malignant tumors detected at an early stage reaches more than 90%.
Types of moles based on benignity
Morphological features of moles provide primary information about their structure and character. The full picture can only be revealed by histological examination. Thus, there are three conditional groups of skin neoplasms:
- Benign neoplasms - nevi.
- Precancerous or borderline - basilioma.
- Malignant - melanoma, skin cancer.
Benign nevi
Widespread. We can say that upon closer examination they can be found in the majority. Such plaques have smooth and clear edges, they can be of different solid colors. They are capable of increasing in size, but this process occurs slowly and often goes unnoticed. Their growth is not associated with discomfort - it does not cause itching or inflammation.
Borderline neoplasms
These include potentially dangerous pigmented formations - atypical moles and basiliomas. When certain conditions are created (trauma, excess sun), they can turn into a malignant form. There is a simple formula - the abbreviation AKORD. With its help, you can try to independently determine the presence of an atypical mole.
A - asymmetry;
K - edges;
O - color;
P—size;
D - dynamics.
An asymmetrical mole with uneven edges of uneven color, changing its size and changing its appearance is atypical.
Malignant structures
Changing the color of a mole
Dermatologists are often approached with the problem of changing the color of a mole.
In most cases, such a change does not mean anything good. Yes, this is not always a sign of the development of cancer, but this does not make the problem any less. As soon as a modified nevus is discovered, you should immediately go to the doctor and make regular visits for routine examinations a common practice. There are many reasons for a mole to change color. Firstly, this may be a consequence of attempts at home lightening or nevus removal. In such cases, you should get diagnosed by a doctor as soon as possible and undergo removal by a surgeon, because home procedures can significantly worsen the condition of the nevus and cause malignant processes of its transformation.
If, in addition to a change in color, there are also unpleasant sensations around the mole, for example, itching and burning, this indicates a high rate of negative reactions in the skin cells, often a reaction to melanoma.
Often a mole changes color after injury or mechanical stress.
This is also accompanied by a change in the shape of the skin formation. The nevus changes shape, size, color, and can also thicken. In the absence of any unpleasant sensations, degeneration can pass completely unnoticed over a long period, for example, several months, or in a matter of days.
The most terrible option is when, with a change in color of the mole, bleeding or suppuration also appears. In this case, you should treat the nevus with hydrogen peroxide at home and go for a consultation with a doctor.
If a mole turns from colorless to brown, this is in most cases a normal process of pigment accumulation under the influence of ultraviolet rays. But for peace of mind, it is still worth contacting an oncologist or dermatologist for a detailed examination and diagnostic procedures, during which you can determine the reasons for the change in color of the nevus.
Signs of a dangerous mole (video)
It’s clear that you can’t touch them - tear them off, pull them with threads, or injure them. You need to be careful if the mole is constantly touched - by clothes, belts, handbags.
READ MORE: Large mole on the back is convex
All your moles need to be examined from time to time, because melanoma often develops from an inconspicuous small mole. Atypical cells begin to multiply there, and even a small malignant tumor on the skin can metastasize and kill a person.
A so-called ABCD test has been developed to help identify the “wrong” mole:
- A - asymmetry. If a beautiful round mole becomes asymmetrical, as if “creeping” across the skin, changing shape, this should be a signal to immediately consult a doctor.
- B - from the English word “border”, which means “edge”. When fuzzy, jagged or blurry edges of a mole appear, this is also a suspicious symptom.
- C - from the English “colour” - “color”. A normal mole has a uniform color - light or dark bronze. If several colors appear (red, white, purple, black), the mole loses the enzyme and becomes heterogeneous - this is also one of the factors that should alert you.
- And finally, D is the diameter. If the diameter of the nevus exceeds six millimeters, it is advisable to see a doctor. In general, if any sign is clearly visible, it is advisable to do a biopsy of the mole - take a small part of it for analysis to identify malignant cells.
- An increase in the size of the mole is more than 7 mm;
- The appearance of a zone of inflammation along the edges of pigmented skin formations;
- Bleeding and itching of pigmented skin formations.
When diagnosing melanoma, it is important to take into account the fact that in men this tumor is most often located on the back, and in women on the lower leg. Regardless, all areas of the skin should be checked, including the scalp and nail beds (melanoma may appear as a black spot under the nail).
If these signs are detected, you should immediately consult a dermatologist. The earlier melanoma is detected, the greater the chance of successful treatment.
A mole that has begun to change color is potentially cancerous. For example, one-color pigmentation has acquired some other spots around or in the middle.
An important feature is a change in the height of the previously flat spot and density (thickening).
The mole hurts, the surface becomes larger, erosions appear, the release of fluid, purulent masses or blood appears.
How to distinguish melanoma from an ordinary mole? Is it possible to recognize a neoplasm on your own? Doctors unanimously say - yes, you can and should be able to do this.
Therefore, experts have developed recommendations that can help you notice the difference between a mole and melanoma. These tips are based on five main features:.
- Problems with asymmetry. Normal moles are completely symmetrical. If you draw an imaginary line through their middle, then the halves should be completely identical. In suspicious cases they are not the same on both sides.
- The edges are blurry. In healthy spots, the border is clear. Degenerating moles have blurry, uneven edges.
- Change of shade. Nevi that are more than one color or have different shades are considered suspicious and should be seen by a doctor. Normal birthmarks are usually one color, but may include light and dark shades of the same color.
- Increase in size. If the spot is larger than the eraser on a pencil, then it should be examined by a doctor. This is also necessary for those spots that do not have any deviations in color, border, or asymmetry.
- If the nevi have changed their number, symmetry, borders, or color, they should be shown to a specialist.
The above signs of degeneration may be accompanied by itching and bleeding.
There can be from one to a hundred moles or more on the human body; their quality and quantity depend on heredity. It is necessary to monitor the nature of the development of moles on the body, as well as the appearance of new ones and, at the first negative symptoms, consult a doctor.
The sun and solarium provoke the development of melanomas - malignant moles.
The mole will definitely need to be removed, but first a biopsy will be performed to determine whether the formation is malignant or benign. This will determine the tactics of further therapy.
Getting rid of moles
In most cases, in case of abnormal changes in the color of moles, the doctor prescribes to the patient a procedure to remove them, and then a histological examination of the biological material obtained during the operation. It is impossible to check a mole with a biopsy before removal, since any mechanical impact on it can become an impetus for the development of melanoma.
Today, there are many methods for removing moles. Each has its own pros and cons, which are important to weigh before making a final choice in favor of one of them.
The cheapest and simplest method is surgery. The skin, previously anesthetized, is excised with a scalpel, and the pigment spot is removed. The whole process takes no more than an hour. The advantages of this operation are low cost, the disadvantages are a long rehabilitation period, the presence of scars.
The most popular and most expensive method is laser exposure. The beam cuts off the nevus in layers, so there are no scars, and the skin heals very quickly. The procedure is performed without anesthesia and lasts only 3 minutes. Its separate advantage is complete bloodlessness and lack of contact with the skin of the device and the surgeon’s hands.
Nevus removal
If your mole changes color, you need to go to the hospital to see a dermatologist. However, in cases where there is no such specialist nearby, contact a dermatologist and oncologist. Surely the doctor will advise you to remove the nevus, after which he will conduct a histological examination of the neoplasm. Doctors can biopsy skin growths, but only if it is not a nevus, otherwise the biopsy is prohibited, because During the collection of material, the skin is injured and this can become a real impetus for the degeneration of the tumor.
Experts do not always advise removing benign tumors, especially if they do not bother you. However, a change in the color of a mole may be a reason to remove the nevus, and as soon as possible. Modern methods of removing pigmented spots leave virtually no marks on the skin, are pain-free, and do not take much time. There are a lot of advantages, so there is no need to worry, especially if you turn to a highly qualified surgeon. What ways can medical clinics offer you to get rid of moles:
- Surgical excision. The most understandable and cheapest method of nevus removal. The skin around the nevus is anesthetized, after which the skin is cut with a scalpel and the pigment spot is removed. The operation takes about an hour depending on the size of the mole;
- Laser removal. The laser beam cuts off the nevus in layers, rarely leaves marks, the skin heals quickly, the operation lasts about 2-3 minutes, is painless even without anesthesia, bloodless and affordable. Suitable for excision of nevi on open areas of the body, including the face;
- Electrocoagulation. To remove a stain, a high-frequency beam of current is directed at it. Cody healing occurs quite quickly, but there is a risk of marks appearing;
- Surgitron. The nevus is removed with a beam of high-frequency radio waves; the method is somewhat reminiscent of a laser. Quite popular and widespread in modern medicine;
- Cryodestruction. Skin cells with pigment are frozen with liquid nitrogen and destroyed. It takes a long time to heal, but there are no consequences in the form of inflammation, although a scar may appear.
In many cases, you can choose the method of nevus removal yourself. The main thing is not to miss the moment when the color of moles begins to change in order to prevent sad consequences as early as possible. Remember: melanoma can take hold of the body very quickly, so you shouldn’t delay treatment, but you shouldn’t turn to traditional medicine due to lack of time. Contact a good clinic for laser removal of a problem spot, where your nevus will be removed in just 5 minutes, and you can return to your business. Think about it: you can get rid of problems and possible cancer in a few minutes during your lunch break or right after work.
Five signs when a mole is becoming dangerous
Scientifically, a mole is called a “nevus” (Latin: Naevus). In serious medical terms, this is a benign pigment formation consisting of special pigment-producing cells (melanocytes). They can be convex or flat. But out of habit, we will simply call them moles.
We asked a dermatovenerologist, oncodermatologist, cosmetologist, director of the aesthetic medicine clinic “Cher ami”, Ph.D., to answer all our questions about them. Irina Aksenenko.
1. Is it bad when there are many moles on the body?
— It’s impossible to say whether this is good or bad. The presence of moles and their number is determined by hereditary factors. If you know all your moles inside out, they remain constantly unchanged, do not grow, do not change color, this is very good.
There are only two reasons for the occurrence of nevi - heredity and exposure to the sun. Excessive sun abuse provokes the appearance and growth of moles. On average, each person may have a different number of moles, but if there are more than 20, you need to closely monitor them. As a rule, all moles are acquired and appear during life.
2. Why does a mole change color?
- Every person should take care of their moles. If it begins to change color or begins to grow, this is a serious reason to consult a doctor. Such moles have a high chance of developing into malignant tumors. And this does not depend on the number of moles on the skin: a person may have only one nevus, but it can be dangerous. And a person with a hundred nevi will be out of the risk zone. Here are a few signs when a mole becomes dangerous:
+ began to grow rapidly - not only is a large mole easier to injure, but it can also grow into a malignant one. In general, any mole larger than 7 mm needs careful monitoring;
+ if hair has fallen out of a mole. You will be surprised, but hairy nevi are a good sign! This means that blood circulation is good and nothing bothers the skin. But if your hair has fallen out suddenly or has never grown at all, this is also a reason to think twice and go to the doctor;
+ the surface became lumpy, uneven, began to bleed from time to time, and became covered with ulcers.
+ when touched or rubbed by clothing, some sensations appeared (pain, tingling), but this had not been noticed before.
3. Are red dots also moles?
— People often confuse viral papillomas (colloquially known as warts), capillary hemangiomas (red spots) and seborrheic keratomas (rough formations on the skin of various sizes) with moles. But they are not even related to each other! The former arise due to a virus, the latter appear due to the interweaving of capillaries, but are also considered benign tumors. And still others arise due to liver dysfunction.
Of course, if they interfere, they can also be removed, just like moles.
4. If you remove them, will there be a trace? And won't they grow again?
- Now there are gentle removal procedures - radio wave and laser, the fastest. The radio wave method is delicate, not rough, with the least heating of the skin. Both of these methods allow you to remove moles within healthy tissue. But of course, the mark will still remain, because the nevus is located not only on the surface, but also in the deeper layers of the skin. Within two to three weeks, a small hole remains at the site of removal, which eventually heals into a barely noticeable scar. If a mole is removed correctly, it will never appear again.
5. Is it always necessary to check removed tissue?
Is it dangerous if a mole is shiny or glossy?
A mole is a benign formation. In both adults and children it comes in several types:
- Flat dark nevus. The most common type of moles. If the spot turns black or a red rim appears around it, this is a signal that can inform about an incipient pathology;
- Convex black mole. A black spot slightly raised above the surface of the skin alarms the owner, so such moles are usually closely monitored, noticing the slightest changes;
- Red-black nevus. It is less common than others and causes concern due to its appearance. Inhomogeneous color does not mean pathology. It is dangerous if a mole suddenly begins to change color: for example, it was reddish and became half black;
- Hanging black moles. Hanging moles should not be black. If the hanging nevus darkens, it means that it has been injured and blood has stopped flowing to it. The mole will gradually dry out and fall off. Experts advise removing dying moles in advance to avoid complications.
A black mole is not dangerous if:
- its diameter does not exceed 5 mm;
- it has clear outlines of an oval, a circle;
- the surface is smooth, repeating the skin pattern;
- the edges are clearly defined and not blurred.
Dangerous are:
- Dysplastic nevus. A black mole localized to any part of the body. Significantly increases the risk of developing melanoma. Signs: a flat mole larger than 5 mm in size, with unclear contours, asymmetrical, has several shades, the central part is raised;
- Melanoma. An ordinary mole that began to change: black, red, blue or white dots appeared, the formation began to resemble a hard lump. The nevus may become discolored, dry, rough, and painful.
Nevi that form after 35 years should also be of concern. Especially black ones, fast growing ones, with jagged edges. You need to undergo examination to avoid complications:
- bleeding moles;
- formation of nodules;
- dysfunction of internal organs: liver, kidneys;
- growth of metastases.
Moles on the skin are a common occurrence. They are located unevenly throughout the body. The nature of the formation should be checked at the moment the shade changes. A sign of possible onset of malignancy. Symptoms also include:
- Rapid growth and drying out.
- The appearance of itching, pain, crust on the surface, microcracks. You cannot scratch a nevus.
- The surface begins to shine unnaturally.
- Blood may ooze from a mole when touched, in a calm state.
- An increase in volume in height, looseness, bumps, and unevenness appear.
- Change or loss of natural skin pattern.
The mole may become filled with blood and burst. The danger is suppuration after scratching. It is strictly forbidden to do this; it is recommended to go to the hospital.
The gloss on the surface of the spot does not necessarily indicate a malignant nature. Depends on external factors and predisposition. Formations should be checked regularly. If the birthmark grows or dries out, this is another signal that an examination is required.
Heterogeneous, multi-colored birthmarks on the body of women, located on the legs, and in men on the torso, head, shoulders, and lower back, more often degenerate into malignant formations. Nevi located in places of permanent injury require special attention.
An alarming signal is a change in the halo around the mole. Papillomas appearing around the area may indicate cancer. At the same time, itching and burning intensify. Normally this shouldn't happen. After tests and other examinations, treatment or removal is prescribed to prevent malignancy.
Uniform age spots often do not pose a threat to human health. They need to be monitored, especially if new growths begin to appear or color changes occur.
We invite you to familiarize yourself with Baking soda: beneficial properties and methods of use, benefits and harms when taken orally
In most cases, if a mole has changed size and shines, this is one of the signs of malignancy. But gloss cannot be called the main and always sure sign of malignancy. It is considered in conjunction with other symptoms.
Malignancy is indicated by the appearance of a glossy surface and a change in color. A two-color mole becomes uneven and bumps appear. Requires a medical examination and examination.
The test results will show whether the shiny, glossy surface of the nevus is an alarming symptom.
Formations on the body are benign in nature. Only modified ones are dangerous.
Alarming nevus transformations:
- changes color to red, brown, white or black;
- increase in volume;
- curvature;
- redness;
- darkening of the skin around the nevus.
With age, changes occur gradually; the number, color and shape of moles slowly changes. Transformations are stable.
Rapid growth and changes in color indicate disturbances in the body and the development of skin cancer. Under the influence of factors, accelerated atypical cell division and transformation into a cancerous tumor occurs.
Education does not immediately begin to turn black. There is a slight darkening, black inclusions and dots appear on the tip. Danger signs requiring immediate action. Pay attention to the situation when the mole turns black and dries out. The appearance of a black nevus is an indirect sign of the onset of degeneration and a reason to visit the clinic. A clear danger is posed by changes in growth, asymmetry of shape in combination with blackness.
Redness of a nevus should be cause for concern. Perhaps an infection has occurred and inflammation has begun. Traumatized formations undergo degeneration. Changes should be examined by a specialist.
You should consult a doctor if symptoms appear:
- itching;
- pain;
- significant changes in size and color;
- rough area around the growth.
Signs of transformation of a benign growth into a malignant tumor. To determine the type of formation, a histological examination is prescribed. If the answer is positive, additional tests are prescribed: MRI, CT, ultrasound. They will help determine the type of tumor, stage, presence of metastases affecting the lymphatic system, distant organs. Surgery is indicated to remove the cancerous tumor. If metastases are detected, chemotherapy and radiation are prescribed.
If the test is negative, the doctor prescribes treatment with tablets, ointments, and gels. It is possible to remove a nevus using the following methods:
- laser therapy;
- freezing with liquid nitrogen;
- radio wave method;
- burning out the build-up using high-frequency current.
Hanging growths located in places subject to frequent injury must be removed. If the mole has changed color or turned black, it may be influenced by sunlight. Removal is optional. If a nevus turns black under clothing, you should get it checked.
You should not self-medicate at home with folk remedies. It will help remove the top layer of the growth, the root will remain in the deep layers of the epidermis, and active cell division will begin, leading to the transformation of the mole into melanoma.
If you look closely at the moles on your body with a magnifying glass and a bright lamp, you can see interesting things. Not a single mole is 100% evenly colored. Some have darker areas in the center, others on the periphery, and others generally have lighter fragments.
You might unwittingly think that you have lived with melanoma all your life and only now noticed it...
Like any part of the human body, a mole does not have perfectly straight lines, identical proportions, or 100% symmetry. In the photo you can see how the pigment melanin, which is produced by the cells of the mole, forms a pigment network. It can be uniform by definition.
In a living organism that is constantly changing, such a situation is impossible in principle. Therefore, the pigment in some moles may be produced unequally, and our eye will see an uneven color.
We suggest you read: Can men take fluconazole for thrush?
Yes, this may be one of the signs of a malignant mole. However, to correctly answer this question, we need to analyze more than just one sign that caught our attention. It is necessary to comprehend all the information about the mole. Long-term existence without any significant changes, absence of asymmetry, bleeding without trauma will be arguments in favor of benignity. If the mole has a slightly uneven color, most likely everything is fine.
On the other hand, the presence of uneven coloring and, for example, rapid growth (more than 1-2 mm per year) or pronounced asymmetry will make any oncologist wary.
If this is the case, most likely we are talking about a dysplastic (atypical) nevus. These nevi are called that way because they often have uneven coloring or an uneven edge. Upon examination, they may resemble melanoma and it can be difficult for a person not associated with oncology to distinguish one from the other.
Read also
How to watch TV for a child: Don’t hang out for more than 30 minutes, don’t come within 3 meters
Rospotrebnadzor has issued a memo for parents on how children can watch TV
Chief oncologist Andrey Kaprin: We have learned to stop tumor growth in 90% of liver cancer patients and save patients with advanced breast cancer
The head of the National Medical Research Center for Radiology told how technologies to combat the “disease of the century” are developing in our country
I dabbled in snus and my heart stopped: a man was saved after a “killer dose” in Krasnodar
Doctors connected him to a heart-lung machine to bring him back to life.
“They cut off the skin from the back”: it will take years to treat a six-month-old girl with the largest birthmark
Almost all hospitals in the country and abroad refused Vika Khvostantseva - and only in St. Petersburg they agreed to operate on the baby for free
Doctors came to the conclusion: the worse the vision, the shorter the life
Scientific and medical data show that eye diseases are one of the important factors on which human life expectancy depends
“He was just unlucky”: a famous doctor explained why oncologist Andrei Pavlenko’s cancer was discovered so late
The disease left no chance for the famous surgeon - and he himself understood this very well [photo, video]
Researchers have named the most dangerous diet for modern humans
This type of nutrition allows you to lose excess weight the fastest, but threatens serious retribution [expert comments]
Bad mood in cloudy weather: lack of sun, depression or reaction of a healthy body
Why do we mope when it’s gloomy and cold outside? Komsomolskaya Pravda talked to an experienced psychiatrist about myths and the truth about the causes of autumn-winter melancholy
Oncologist Nikolai Zhukov: More and more people, faced with cancer, remain alive
Head of Department of the National Medical Research Center named after. Dmitry Rogachev told what is important for patients, their relatives and all of us to know so as not to fall into panic and despair
In Tuva, neurosurgeons saved an 8-year-old boy by fixing his spine broken in an accident with screws
The child is already on the mend
Top 5 discoveries in the fight against aging: do not deprive yourself of carbohydrates, relax and wait for a cure for old age to appear soon
Alexander Tyshkovsky, a researcher at Harvard Medical School and Moscow State University, spoke about the main scientific achievements and prospects for extending healthy life to KP [video]
New life in 2020: leading scientists and doctors told how to become slimmer, smarter and younger
For advice, we turned to a longevity researcher, a neurologist, a cardiologist, an endocrinologist, a sleep specialist and an oncologist.
Alcohol: how to mix without shaking
The toxicologist sorted it out. What is the safest way to combine different types of alcohol?
Sleeping on a winter night: scientists have proven that you can actually get some sleep on weekends and holidays
A major study will delight everyone who plans to spend a considerable part of the New Year holidays in the arms of Morpheus
Long holidays: 5 tips to make the most of them
Do you want to sleep during the holidays? Or have a blast? How to spend time profitably and not ruin your holidays with sudden illness, experts suggest
“I must live for the sake of the children”: due to a doctor’s mistake, the mother of 6 children is struggling with stage 4 cancer
Only at the age of 36 Indira learned that she was seriously ill [kp.ru exclusive]
Drinking is not a cure: a toxicologist named medications that should absolutely not be combined with alcohol
On the eve of New Year's feasts, "KP" learned from an expert which drugs for the treatment of the most common diseases should never be combined with alcohol.
How can we get closer to global healthcare standards?
A national certificate “Quality and safety of medical activities” has been introduced in Russia. These and other issues were discussed at the Russian Healthcare Week forum.
What are the risks for women with silicone implants: the surgeon explained when to go to the doctor
The doctor suggested what could have caused Lera Kudryavtseva’s illness
A passport is not an argument: How I tested the first biological age calculator created by Russian scientists
The kp.ru correspondent went through the research procedure from start to finish and found out whether the numbers in the passport differ from the state of the body
Lemon is not a friend to cognac, and fatty meat should be washed down with dry wine
A nutritionist spoke about suitable and inappropriate food combinations on the New Year's table
"Russian Healthcare Week": new forms for familiar drugs
More than 1,000 companies from 40 countries took part. At the PharmMedProm-2019 forum, new drugs were discussed, Russian developments and generics were presented
Science Proven: How Much Water You Really Need to Drink
An endocrinologist told how to determine your individual water consumption rate
New Year's miracle: Russian doctors saved a 7-month-old girl with a heart tumor
For the first time in our country, a unique operation was performed by cardiac surgeons from the St. Petersburg State Pediatric University
Eat a fur coat and fit into a dress: how to lighten the calorie content of holiday dishes and not deprive yourself of pleasure
What are the pros and cons of traditional New Year's dishes, says a nutritionist at the Institute of Personalized Medicine of Sechenov University
Hit women on the shoulders, men on the withers: how to steam properly and what to drink in the bathhouse
On the eve of the New Year, Komsomolskaya Pravda journalists learned from a professional steam cleaner how to relax in a bathhouse in order to be happy and healthy
Why do nevi change color?
The color of moles depends on the work of melanocytes, which produce melanin. Excessive accumulation of skin pigment leads to darkening of the formation, and insufficient accumulation leads to lightening . Such changes are observed under the influence of the following factors:
- Ultraviolet. Sunlight and radiation in a solarium promote the proliferation of melanocytes. Therefore, after too intense exposure to ultraviolet radiation on the skin, moles may darken or their total number may increase. Due to the influence of this factor, the risk of malignant degeneration of nevi increases significantly.
- Hormonal imbalance. Moles can change their color during puberty, pregnancy, and the onset of menopause.
- Injury. A mole may turn black after being damaged by friction with clothing or a cut with a razor.
- Skin diseases. The nevus becomes black or colorless if a person suffers from inflammatory processes affecting the epidermis.
What are angiomas?
Depending on the type of vessel that caused the neoplasm, the following types of angiomas are distinguished: capillary, venous, arterial. Based on the depth of their location in the skin, flat and convex angiomas are distinguished.
| View | Description |
| Flat | Moles that do not rise above the top layer of skin |
| Branched | A pulsating, convex mass filled with blood. When pressed, it turns pale, then turns purple again. |
| Pineal | Convex spherical moles |
| Arachnids (stellate) | Moles from which a network of thin blood vessels arises |
| Knotty | Tumor-like, well-defined neoplasms of burgundy-violet color. Often localized on the wings of the nose, in the corners of the lips and other parts of the face |
| Cavernous | Several angiomas located in a chain one after another. Often localized on the face, which significantly spoils the appearance |
Types of angiomas
The main danger that red tumors pose is their ability to change their character to malignant. Changes can be triggered by several factors: due to mechanical damage, as a result of exposure to ultraviolet rays.
Angiomas
Red moles located near the nasal passages and near the corners of the eyes often cause disturbances in visual and olfactory function. This is especially true for children.
- Careful handling of the mole, protection from mechanical influences.
- Drink at least two liters of fluid per day.
- Including foods rich in vitamins E and D in your diet. For example, avocados and olive oil.
- Regular bowel cleansing. You can eat spirulina algae, which removes toxins from the gastrointestinal tract.
- Protect yourself from excessive exposure to ultraviolet rays. This is especially true for white-skinned people with red or blond hair. If you stay in the sun for a long time, you must use sunscreen.
- Moisturize skin as needed.
Red moles on the body are usually not dangerous. They are benign formations. You should consult a doctor only if the angioma causes discomfort or spoils the aesthetic appearance. Modern medicine offers several quick and painless ways to get rid of this disease.
If a single angioma or multiple neoplasms are detected on the body, a woman is advised to consult a specialist. He will conduct a full examination and determine whether the mole needs to be removed.
We suggest you familiarize yourself with How to remove capillaries on the face, red capillaries have appeared
| Method | Description |
| General examination and interview of the patient | The specialist examines the neoplasm, the skin around it, and determines the time of appearance of the mole |
| Clinical blood test, biochemical blood test | Analyzes make it possible to identify abnormalities in the internal organ systems that could cause angiomas |
| MRI | This type of diagnosis is not always indicated; it is most often required when identifying signs of a tumor of internal organs. During the procedure, the specialist can see even a small tumor |
| Biopsy | It is prescribed for pain, discomfort and rapid growth of a mole. The doctor takes a sample of material that is examined in the laboratory |
After receiving the results of the examination, the doctor will determine whether removal is necessary and the best method suitable for the patient. Sometimes an additional ultrasound examination is required to identify diseases of the internal organs, as well as studying the woman’s hormonal levels by taking a blood sample and sending it to the laboratory.
When such a formation appears on the skin, it causes some discomfort, but is not dangerous to health. In their shape, angiomas are similar to an asterisk or spider; they can be punctate or cavernous. The latter are located very close to each other, so from afar they can resemble a cave.
Based on the tissue composition, angiomas come in several types:
- flat;
- in the form of cones;
- knotty;
- branched.
The appearance of angiomas is not in itself a prescription for their removal. If moles do not change size and do not cause pain or discomfort, then there is no need to remove them.
Watch the video that explains when you need to see a doctor
The signal to seek medical advice is:
- A sharp increase in the number of angiomas. Many red moles localized in one area are a sign of ill health;
- Increase in the size of the nevus in a short period of time, sharp growth;
- Asymmetrical shape, unclear contour of the mole;
- Convex angioma, which is injured by clothing, a comb;
- Formations that cause pain and severe discomfort
During pregnancy
Risk factors
A dark or colorless mole is prone to malignant degeneration when exposed to the following unfavorable factors:
- Excessive insolation. A nevus can change its color and become malignant if it is exposed to maximum solar radiation for a long time.
- People with fair skin and hair and blue eyes are most likely to develop skin cancer.
- People with a large number of moles - more than 50.
- The presence of a large nevus on the body, the diameter of which exceeds 6 mm.
- Bad heredity. This is one of the most common causes of oncology due to the transmission of defective genes from parents to children.
- The presence of dysplastic nevi on the body. They are characterized by a vague outline, irregular shape and slight elevation above the main surface.
- Frequent inflammatory processes on the skin near the mole. At risk are people who have suffered from dermatitis, psoriasis, and eczema for a long time.
- Localization of the nevus in a place where it is subject to friction with clothing or is easily injured.
If a person observes the presence of one or more unfavorable factors, this does not mean that he will develop skin cancer. They only indicate an increased likelihood of such an unfavorable outcome.
Risk group
Scientists identify certain risk factors for the degeneration of pigmented nevus into melanoma.
These include:
- people with very white skin, prone to developing sunburn (phototypes I - II);
- the presence of multiple freckles and moles on the skin;
- patients with a hereditary predisposition to the development of melanoma (disease in close relatives);
- the appearance of a large number of moles on the body at a certain period of life (which is most dangerous in old age);
- prolonged exposure to active solar radiation on the skin;
- constant mechanical impact and traumatization of moles (when scratching, if the mole is located on the head or when shaving with a nevus localized on the cheek);
- patients with benign skin tumors or atypical nevi (melanoma-dangerous moles);
- changes in the size and structure of nevi;
- re-growth and change in the appearance of the mole after removal.
When danger arises
Moles appear throughout a person’s life (most of all in the first twenty years). This process occurs in everyone and does not pose any danger. Moles can be small, occupy a fairly large area, be flat, or rise above the body. All such formations have approximately the same chances of malignant degeneration.
Hanging nevi are especially dangerous. They are attached to the surface of the epidermis by a thin stalk. Therefore, they are easily injured, which can become an impetus for the development of oncology.
If at some point in life a mole has changed, you need to pay attention to signs indicating the onset of a malignant process:
- the mole has suddenly changed color to a darker or lighter color,
- the hanging nevus suddenly turned black and fell off (this happens due to the breakage of a thin stalk),
- the surface of the formation dries out and cracks,
- the mole has increased significantly in size,
- the nevus provoked the appearance of uncomfortable sensations - pain, burning, itching,
- the structure of the skin formation has changed - it has become convex, bumpy,
- the nevus acquired unclear boundaries, became asymmetrical,
- any liquid is released from the surface of the growth,
- the skin around has darkened or turned white, and a characteristic rim (halo) has appeared.
What to do
If a mole changes color, you need to see a doctor to determine the cause of this transformation. Sometimes this is completely normal and does not indicate the development of cancer.
If there are direct signs of malignant pathology, removal is mandatory. The collected biological material is sent for histological examination, which helps to establish an accurate diagnosis. When cancer is confirmed, the patient is prescribed appropriate treatment.
Surgery is indicated if the mole has darkened or turned white and is located in places that are constantly exposed to injury. This decision will reduce the likelihood of an unfavorable outcome.
Removing normal moles for aesthetic reasons is undesirable, since the intervention can provoke more serious consequences.
Removal methods
If the nevus turns pale, darkened, or becomes covered with suspicious bumps, doctors recommend removing it.
This can happen in several ways:
- Excision using a scalpel. The method is widely used in cases of suspected cancer. The collected biomaterial is sent for detailed examination, which allows an accurate diagnosis to be made. The disadvantage of this method is the high level of tissue trauma, which increases the postoperative recovery period.
- Laser destruction. Acceptable when identifying small formations. After its use, there are no scars left on the body, and the recovery period is minimal. The disadvantage of the procedure is the impossibility of completely eliminating the formation, which sometimes leads to its re-growth.
- Radio wave destruction. Removal of skin growths occurs with minimal blood loss, since blood vessels are cauterized during the procedure. When exposed to radio waves, only nevus cells are destroyed, and healthy tissue is not affected. The method is effective, but is not used for large tumor sizes.
- Electrocoagulation. Removal is carried out using current. During the procedure, the level of blood loss due to capillary coagulation is reduced.
- Cryodestruction. The technique is used to eliminate small superficial formations on the body. The procedure takes place under the influence of liquid nitrogen.
Diagnostics
Dermatologists and oncologists are involved in determining the type of nevus.
Using a dermatoscope, the doctor examines the formation and determines its nature (benign or malignant). Sometimes a histological examination (scraping method) is required.
Biopsy (tissue sampling) for nevi is not used due to their trauma during this procedure. And as you know, it’s better not to touch moles again!
The exact causes of a red mole have not been established, but methods for its diagnosis and treatment have been developed at a high level.
Types of examination to establish the correct diagnosis:
- Taking an anamnesis - the doctor asks questions about the existence of a similar mole among the patient’s family members, about the possible reasons for its appearance and changes;
- Referral to a more specialized specialist - dermatologist, surgeon, oncologist, endocrinologist, gastroenterologist, neurologist;
- Dermatoscopy – the doctor conducts an external examination of the birthmark;
- Digital dermatoscopy is a digital image of a mole taken using a dermatoscope and displayed on a computer screen. The possibility of such magnification and examination of the birthmark simplifies the study;
- Biopsy is a method for diagnosing malignant neoplasms; if this procedure is carried out correctly, the result is 100%. Types of biopsy: Puncture - a piece of tissue is taken with a needle in a limited amount under anesthesia;
- Total excision is also a therapeutic procedure in which tumors are removed or used for histological testing;
- Histological test - study of the structure and possible changes in tissue at the cellular level, under a microscope (the most important, final type of diagnosis);
- Additional studies in case of suspected melanoma - a malignant tumor:
Even a doctor with extensive professional experience cannot always identify the process of degeneration of a tumor into malignant at an early stage. This is the main reason for performing a biopsy and subsequent histological analysis.
Sometimes computer dermatoscopy of pink moles may be required - the latest technique to diagnose degeneration. With its help, you can not only look at superficial changes, but also see what is happening more deeply.
We suggest you familiarize yourself with Fungus between the toes: symptoms and treatment
In this case, the tissues are not injured. The obtained data is transmitted to the attending physician, who analyzes it and determines the degree of risk.
Only after this does he prescribe treatment or make a radical decision to remove the mole.
This diagnosis is carried out to determine whether malignant cells are present in the tumor. For this purpose, they are removed and sent for further biopsy - a study that allows for an accurate diagnosis.
Examination is also possible using a dermatoscope - the device detects malignant growths at an early stage.
When visiting a doctor, a person will have to undergo a series of tests to determine the type of mole and understand the risks of its degeneration into melanoma. To do this, perform the following manipulations:
- the doctor conducts a conversation and finds out when the mole formed and whether it caused discomfort or pain;
- examination of the nevus under a special lamp - a specialist will evaluate the structure of the tissues and characterize the surface of the formation;
- performing scraping from the surface of the mole.
If necessary, a biopsy will be prescribed - the removal of a small fragment of nevus tissue for histological examination. This is the most informative method for diagnosing malignant tumors.
How to prevent malignant degeneration
To prevent the development of oncological processes in moles, you must adhere to simple rules:
- Removal of nevi and other skin growths should only occur under the supervision of a physician using safe methods. Self-treatment of such formations is extremely undesirable.
- It is necessary to prevent injury to moles. If the risk of damage is high, it is recommended to consult a doctor to remove the formation surgically.
- If hair grows on the surface of the mole, you should not pluck it with tweezers. It's best to simply cut off the excess with nail scissors.
- It is not recommended to apply cosmetics to the surface of nevi; this may lead to an unpredictable reaction from the body.
- The surface of the skin with moles should be protected from all negative external influences - the sun, chemicals, friction.
With the right approach to the problem, the risk of an unfavorable outcome is significantly reduced. Therefore, darkened nevi require special attention and, if necessary, treatment, which should only be carried out under the supervision of an experienced doctor .
Why do they appear?
Nevi are essentially benign skin formations.
Some people get scared when they see many moles on their body. What does this mean for a specialist? Only that the patient’s body is prone to accumulation (accumulation) of melanin in the surface layers of the epidermis.
1. External:
- exposure to ultraviolet radiation, one of the most common factors in the formation of moles due to increased melanin levels during tanning;
- traumatic damage to the epidermis, systematic violations of the integrity of the skin contribute to the appearance of pathological changes in it;
- exposure to radiation, which rapidly changes normal skin cells;
- consumption of harmful products (GMOs, fast food, alcohol) and smoking, these habits negatively affect metabolic processes in the body.
2. Internal:
- endocrine disorders and diseases, any changes in hormonal levels can cause the appearance of skin pathologies, pigmentation, moles;
- hereditary predisposition, the presence of various nevi in the family.
The appearance of moles can be triggered by inflammatory and autoimmune skin diseases, toxic lesions, burns and frostbite, as well as the constant use of low-quality cosmetics and preparations for face and body care.
Every person has moles on their body, but, interestingly, we are often born with clear skin, and acquire these marks throughout our lives. Their location may indicate some problems in the development of the body. In the first two years of life, a person develops very few moles, and they are quite pale, so no one, as a rule, pays much attention to them.
Their main quantity appears at the very beginning of puberty - hormonal imbalances in the body lead to unstable production of melanin, which manifests itself as dark marks on our body. By the way, this is why women can develop a large number of spots on their skin during the entire period of pregnancy.
INTERESTING! It also happens that moles disappear - during an acute deficiency of melanin, the cells of the mole can begin to give it away and, as a result, become lighter.
It happens that a person, looking at his reflection in the mirror, notices the appearance of strange red spots. Of course, the first thought is that these are some kind of skin problems, rashes, allergies or pimples. But pimples manifest themselves in a fairly short period of time: unpleasant sensations come, it is felt that the process is somehow developing (the inflamed area may be a little warmer to the touch).
We invite you to familiarize yourself with Brown spots on the body: photos, causes, treatment
In the case of a mole, such sensations are completely absent, and all the manipulations that girls perform in a situation with a pimple can be disastrous. Many people wonder why red moles appear? They are also called spider veins and hemangiomas, and their appearance can be a warning sign.
IMPORTANT! Red moles can be an important signal from your body. Quite often, the accumulation of red moles in one part of the body indicates a predisposition to cancerous tumors in this particular organ.
What are red moles? Unlike black and brown moles, hemangioma is a vascular benign tumor that can have a small, distinct red dot shape, be slightly protruding, or be quite large in size and visually uneven edges (there are characteristic red threads resembling rays).
Such a red mole is called a stellate or spider-shaped hemangioma, and the mole that has a clearer outline is a punctate hematoma. Also, this tumor tends to manifest itself en masse: several neoplasms can fit tightly together and eventually merge into one tumor.
The color can vary from light red to dark purple. The size also varies: a mole can be a barely noticeable point, or it can grow into a large spot several centimeters in diameter. Typically, formations of this type are classified as cavernous and cavernous moles. However, no matter what shape and color they have, tumors of this type have one characteristic feature: if you press on it with your finger, it will lighten for a while, and then return to its original color.
They arise regardless of anything. This type of tumor affects people of both sexes and all ages, even newborn babies. If there are no specific problems (the education does not cause inconvenience, it is located in a problem-free place), then there is nothing to worry about; in children, such moles go away on their own.
And yet, the decision to remove it should be entrusted to a qualified doctor, because only he will be able to analyze the general condition of the body. Of course, medical examinations require some expenses, but on the other hand, the skin is our largest and most vulnerable organ, which comes into contact with a variety of irritants every day. Therefore, you should treat it with more than care.
The appearance of red moles in adulthood may be associated with the following types of diseases:
- dysfunction of any internal organs;
- long exposure to direct sunlight;
- hormonal imbalances.
If you decide to find out what the reasons for the appearance of red moles are, then you first need to examine the body for hidden chronic diseases that have caused such a problem as collateral damage. In this regard, you should under no circumstances open the tumor yourself: you will damage the blood vessels, and the size of the spot will only increase.
You should also take into account the fact that if such a mole is irritated by any mechanical means, it may well develop from a small benign lump into a closed complex organism, which can become a serious oncological problem. It is a mistake to assume that a small red spot on your skin is the entire cavity of the hemangioma; usually it is only a small part that has come out. If you try to remove such a formation yourself, you can cause bleeding, which is likely to be quite serious.
The need for removal may arise in completely different cases, such as:
- itching;
- burning;
- rash;
- increase in the number of formations;
- pregnancy.
In cases where the mole is located where clothes constantly touch and rub against it, you should immediately visit a doctor. The reason for removal can also be a significant increase in the mole, the merging of several spots into one. All this may indicate the development of various oncological diseases, and tumors can be both benign and malignant. Taking hormonal contraception can also provoke an increase in the number of red moles.
Important Notes
If necessary, histological tests are performed to determine the type of tumor. If the formation is benign, it is removed using a laser; this method is useless, safe and effective. If the size is initially small, then in the future there will not even be a scar left. In order to make the healing process faster, you should follow all the instructions of the dermato-oncologist.
FORBIDDEN! You should not self-medicate; careless treatment of a red mole can lead to serious oncological consequences.
In fact, medicine cannot answer the question of why red moles appear on the body. Nevi can be a consequence of lipid metabolism disorders in the body or a simple dermatological pathology. In order to determine the exact cause, you should contact a qualified professional.
Skin diseases require special attention, so you should not let the process take its course, and even more so, you should not self-medicate. It is important to remember that any disease can be most successfully and effectively treated at an early stage, when the disease is in its infancy. In this case, treatment will be as fast as possible and much less expensive.