Considering the increase in the incidence of melanoma in recent years, diagnosing and determining the risk of degeneration of moles on the body is increasing its relevance in oncodermatology. Every person should monitor their moles, and especially have information about the dangerous signs of changes in the structure of the nevus. One of the parameters for dynamic monitoring of pigment formations is the state of their surface. If a mole peels off, cracks and crusts appear on it, these signs are considered unfavorable and are a reason to immediately consult a doctor.
Why does a mole peel off?
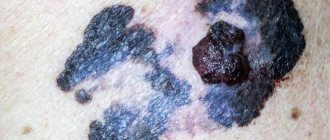
photo of a flaky mole
The surface of the pigment spot is formed by the same epithelial tissue as the surrounding healthy skin. But, unlike skin without birthmarks, the epidermis of a nevus contains a large number of pigment cells - melanocytes, which produce melanin. Pigment products have an exclusively protective mechanism of action for the human body. The melanin layer in the skin reflects and scatters ultraviolet rays, which have a mutagenic effect on cells.
Since the mole concentrates a maximum of melanocytes in its thickness, it becomes the epicenter of the adverse effects of various factors. A nevus is a vulnerable spot on the human skin.
The fact of peeling is not always considered a sign of change or degeneration. If the nevus has been subjected to a sharp impact of an environmental factor, then the mole may peel off temporarily and have no consequences afterwards.
The reasons for the peeling of the surface of the nevus lie in the influence of external and internal factors.
Causes
The causes of peeling nevi in adults, children and adolescents are divided into external and those occurring inside the human body.
External causes of peeling include:
- Exposure to the sun. This is one of the most common factors influencing changes in the surface layer of an age spot. If a mole begins to peel off due to overheating, this is a process of natural change of epithelium. The color does not change, the shape remains convex or flat as it was originally. It is recommended to protect the nevus from prolonged exposure to direct sunlight.
- The influence of ultraviolet radiation when visiting a solarium. After the procedure, the mole may begin to peel off, since the impact of UV radiation with artificial tanning is much stronger than with natural tanning. If the spot remains rough and continues to peel for a long time, you should consult a dermatologist.
- Aggressive exposure to caustic chemicals. If chemicals come into contact with the surface of the nevus, irritation or burns may occur.
- Allergy to components of cosmetic products. This applies to cosmetics that cause dry skin, and is also important for people with severe allergic reactions. In addition to peeling, allergies may cause local tissue swelling and itching (scalp, face). After 14 days, the rough layer should recover.
- Exposure to X-rays. Changing the surface is possible after taking multiple pictures during the examination.
- Mechanical injuries. Constant friction can cause irritation or damage to the mole, and then peeling off its upper covers.
It is necessary to reduce the impact of foreign factors on the surface of the mole . This is especially true for large and convex nevi. Reasons related to internal processes of the body include:
- Phenotype. If a person has a light color of eyes, skin and hair, and there are a large number of moles on the body, then he belongs to a group at increased risk of degeneration of nevi. Changes in color (the spot becomes a darker color), texture (the skin cracks or peels) or size are a good reason to visit a dermatologist.
- Age exceeding 50 years. Due to changes in hormonal balance in a person, the structure of nevi may change.
- Immunity. Significant decrease in immune defense due to previous diseases or active phases of chronic diseases.
- Smoking and drinking large amounts of alcohol. Toxic substances negatively affect the entire human body, including the condition of the skin.
- Congenital predisposition. Hereditary changes increase the likelihood of malignant transformation.
If a pigment spot cracks, bleeds, enlarges or changes color, this is a reason to consult an oncologist as soon as possible for timely diagnosis and treatment.
Signs of degeneration of a mole do not always appear together. Often only one or two may be noticed, but severe discomfort or a significant change in the appearance of the skin should not go unnoticed.
External factors leading to peeling of a mole
- Prolonged exposure to open sun. The natural reaction of the skin in response to insolation is hyperemia, followed by excessive keratinization and peeling. The causes of peeling in this case are dead skin epithelium, which gradually sloughs off and is replaced by a new layer of cells. In this case, the surface of the mole does not change. It still grows hair and has either a warty or flat appearance. The color of the halo and surrounding skin is not changed. There are no unpleasant sensations in the area of the tumor. Itching is possible if preceded by sunburn. Such peeling of a mole does not pose a danger to humans, but since any birthmark can degenerate, it is worth carefully monitoring it in the future. If peeling does not go away for a long time, you should consult a dermatologist or oncologist to decide whether to remove the tumor.
- Tanning obtained artificially - in a solarium. It is known that to obtain the same shade of tan in the sun and in a solarium, different times are required. A solarium requires much less time, but this is achieved by increasing the dose of ultraviolet radiation. In this case, the same changes are observed on the skin and moles as when exposed to natural sunlight.
- Chemical effects on the skin of substances that have a local irritant effect. The reasons for peeling of a mole in this case are a consequence of a chemical burn. Such substances include alcohols, acids, alkalis, fuels and lubricants, solvents, paints, acetone, and resins. Some cosmetics can also cause the mole to peel. Especially for people who are prone to allergies. In such situations, swelling of the skin, hyperemia, and itching are observed. Next, the mole or age spot peels off. After 2 weeks from the moment of exposure to the chemical, all changes on the surface of birthmarks should disappear on their own. If this does not happen, then you should visit a doctor. This tumor may need to be removed.
- X-ray radiation. If for some reason the patient has had several x-rays taken (fractures), then the skin, and especially the moles on it, may begin to peel off. In a healthy person, such a change will pass without leaving a trace. If DNA molecules are not repaired when exposed to ionizing radiation, then after a few years the formation may begin the process of degeneration.
- Mechanical injuries. If a mole peels off after constant friction on the surface of clothes, belts, straps, then you should think about removing it. Constant traumatization of the nevus can lead to degeneration and development of melanoma.
Causes of peeling
Over the course of a person's entire life, many marks and birthmarks appear on the human body. It is not the marks that are dangerous, but their changes in size, structure and shape. If the nevus begins to peel off and dry out, it is quite possible that the process of degeneration of a benign formation into a malignant tumor has begun, accompanied by symptoms:
- pain when touched;
- peeling off the upper cellular layer of the skin piece by piece;
- ring-shaped swelling around the formation;
- detachment of the crust leads to the appearance of a poorly healing wound with the release of pus or white fluid;
- neoplasm, the area around it may turn black;
- growth of a flat mole is observed.
In normal condition, the formation should be soft, smooth, and not compacted to the touch. If symptoms appear, you should consult a dermatologist to identify the causes of the changes. If degeneration is confirmed, you need to contact an oncologist.
A mole dries under the influence of external and internal factors caused by the following reasons:
- abuse of ultraviolet rays. Heavy tanning in the open sun, frequent visits to the solarium lead to the fact that the nevus begins to dry out. Regardless of where the birthmark is located, on the head or leg, the sun's rays are merciless to formations on the skin. White moles should be protected, as they quickly succumb to tanning and may darken;
- causing injury. Dangerous are hanging growths, which often cling to clothing and jewelry, become twisted, and fall off. When rubbed with clothing, the nevus becomes covered with a thin crust, which cracks and itches. You cannot undermine the edge of the scab or scratch the formation; there is a risk of infection, which complicates recovery;
- The growth may dry out due to impaired blood circulation. Poor nutrition leads to drying out of the new growth, which can crumble or fall off;
- allergic reaction to household chemicals, low-quality cosmetics. This leads to irritation of the skin on the face and other parts of the body with which there was contact. The skin will crack and begin to itch;
- the negative impact of radiation during an X-ray or CT scan affects convex, flat birthmarks, causing increased growth;
- due to hormonal disorders during puberty, pregnancy and menopause. Changes in the background lead to drying out of old and new papillomas.
- the process of transformation into a malignant tumor is accompanied by signs of peeling and peeling of the upper edge.
These signs cause discomfort, a feeling of dryness of the growth itself and the area around it.
If itching and peeling of the surface of a mole occurs, but it does not grow, has not changed in color or changed shape, do not panic at this stage. The situation can be triggered by rubbing the nevus with items of clothing, mechanical damage, or the body's reactions to chemicals.
The skin around birthmarks is very sensitive, so the area may become inflamed, red and itchy. It is important to remember what action preceded the onset of itching. The most common reasons include:
- Rubbing a mole, if it is localized in the neck, with a shirt collar, tie, etc.
- Disturbance of a birthmark located on the head during combing, cutting, or chemical dyeing.
- The location of the nevus in the folds of the skin (in the axillary and groin areas) itself carries a risk of injury. In these places, the skin sweats more often, and irritation occurs due to close contact with clothing.
- Men should be careful when shaving if the mole is located in the facial area.
- One of the reasons why a mole on the back or stomach itches is the use of a hard washcloth while taking a shower. Moles in the area of the shoulder blades can also be irritated by chafing underwear straps or backpack straps.
To avoid irritation, choose loose-fitting clothing with straight seams and without the use of synthetic dyes for patterns. The item of clothing should be comfortable and in size. But not only external mechanical influences can cause a mole and the area around it to itch.
Other factors include:
- Allergic reactions caused by poor diet and taking hormonal medications.
- Weakened immunity.
- Insect bites.
- Skin diseases (eczema, scabs, dermatitis). With such diseases, not one, but several moles may itch and grow at once.
- Hormonal fluctuations during adolescence, pregnancy and menopause. The main sign of hormonal imbalance is increased sweating. It is advisable to undergo examination by an endocrinologist to eliminate the symptoms of hyperhidrosis. Personal sweat, mixing with sebum and dirt, irritates pigmented growths.
- Prolonged exposure to the sun.
They try to protect the skin from excess ultraviolet radiation. In summer, exposed areas of the body are lubricated with a protective agent. This also applies to artificial tanning obtained from visiting solariums. The time spent in the booth should be limited to 3-7 minutes. For a horizontal solarium, the safe time is 7 minutes.
Itching of pigmented areas often occurs in people suffering from allergies. Allergy sufferers have more sensitive skin. To relieve irritation, it is enough to take an antihistamine (Loratadine, Claritin). If the degree of irritation decreases, then the reaction is caused by chemicals, food or cosmetics. When the mole continues to itch, you should consult a dermatologist.
If moles itch on your body and there is no explainable reason for this, you should carefully examine the area of skin. Perhaps the birthmark has entered the stage of malignancy - the transformation of benign cells into malignant ones.
Experts have identified a unified system for determining malignant tissue transformation (ABCDE). Its criteria are:
- A - asymmetrical form of education. Benign nevi have a symmetrically limited area.
- B - a dangerous mole has uneven and blurred boundaries.
- C - malignant formations have an uneven color, combining multi-colored shades.
- D - a mole can increase to an impressive size; exceeding a diameter of 8 mm is considered pathological.
- E - the structure of the nevus changes.
The defining signs of tissue malignancy are:
- The appearance of white growths on the surface of the mole, the skin is very itchy and flaky.
- The skin around the nevus is red.
- The birthmark changes color and becomes dark.
- The shape of the formation takes on an asymmetrical appearance with blurry edges.
- The pigment growth increases in size.
- Tissue pain and bleeding occurs.
- In the center of the spot, dark and red blotches, dots, stripes, and sometimes purulent masses or blood fluid form.
- Against the background of an itchy pigment spot, many small nevi form. These pigments also itch and hurt.
When the neoplasm has the listed symptoms, the mole hurts, or a tingling sensation is felt, you should immediately consult a dermatologist to exclude the possibility of developing melanoma, a cancerous skin tumor.
Pigment spots can be congenital or acquired. Congenital ones are harmless. If moles itch and peel, degeneration begins and serves as a reason to remove the stain.
There are up to 30 spots of varying sizes on the body, which is considered normal. The formations differ in melanin content, the pigment gives an individual color. It can be red, beige, bluish, and sometimes the area becomes flat and black. Acquired spots appear during hormonal imbalance, due to genetic predisposition, from prolonged exposure to the sun.
According to doctors, every nevus present on the body, under the influence of certain factors, can transform into melanoma. Melanoma is a malignant tumor. If its appearance changes, attention should be paid to the nevus; it may degenerate into a malignant tumor. People with fair skin are mostly affected by the problem.
Peeling moles are considered dangerous. The process of transition to malignancy is influenced by external and internal factors.
External factors
- Sun. The head is a dangerous zone for the development of melanomas; the cancer cell begins to actively react to dryness and exposure to the sun. If you are exposed to the rays for a long time, the skin exhibits a protective function and the cover begins to peel off. The reason for the process is the necrosis of the epithelium, which peels off over time and is replaced by a new layer of cells.
- Artificial tan, obtained in a solarium. The tanning time is reduced due to an increase in ultraviolet radiation.
- Chemistry. The skin is exposed to substances that cause irritation. The stain may peel off from a chemical burn. Substances include alcohol, alkali, acids, solvents, paints, acetone and resins. Cosmetics contain such components, peeling begins from use.
- Radiation from X-rays. Peeling begins if several photographs are taken for certain reasons. If the patient is completely healthy, it will not affect the skin condition.
- Mechanical damage. If you are regularly exposed to friction against the surface of clothing or a belt, consider removing the nevus.
Internal factors
- Type of skin. Skin type at birth influences the subsequent outcome of spots. If a person is born with fair skin and blue or green eyes, they are at risk of developing melanoma. It is recommended to contact an oncologist.
- Age. After 50 years, a complex change occurs in the body, the aging process intensifies, and organs are more susceptible to cancer. If peeling continues for several weeks, you should consult a specialist to remove the formation.
- Reduced immunity. Occurs for a variety of reasons and can contribute to changes in education.
- Tobacco smoking. Reduces the body's defenses, which increases the risk of stain degeneration.
- Genetics. When the gene responsible for destroying atypical cells changes, cancer cells multiply, and subsequently the moles flake and flake off.
Internal causes that contribute to peeling of moles
- Skin type, or rather, types 1 and 2. The congenital type of human skin largely determines the outcome of all birthmarks and neoplasms. White, light skin, blue or green eyes, light brown hair color - owners of this color type with a large number of moles on the body are at high risk for developing melanoma. If a mole begins to peel off and you have the above color type, then you should immediately visit an oncologist. In this case, the skin has a low level of natural protection and nevi on it are susceptible to degeneration as soon as possible from the onset of changes.
- Age over 50 years. Given the complex age-related changes that occur during aging of the human body, all organs are at risk of developing cancer. Leather is no exception. Melanoma develops in such individuals much more often, especially in women. If a mole has been peeling off for a long period of time, then you need to visit an oncologist to have the tumor removed as quickly as possible.
- Decreased immunity. The reasons for the suppression of the body’s immune forces are different and lie in the presence of diseases: chronic infectious diseases, oncological processes, pathology of the endocrine system. Taking corticosteroids also suppresses the immune system. Any changes in the surface of the nevus, be it ulceration, peeling, cracks, should be a reason for an early visit to the doctor. If there is a concomitant pathology, a mole that has begun to peel off is removed.
- Smoking contributes to the degeneration of nevi into melanoma, so a sign on the surface of a mole, such as peeling, is a reason to remove the neoplasm.
- Hereditary predisposition. A mutation in the gene responsible for destroying atypical cells in the body leads to intensive proliferation of cancer cells. Therefore, any changes on the surface of a mole in people who have relatives who died of skin cancer are a reason to consult a doctor. If the nevus peels off, it must be removed.
Prevention
To avoid peeling of moles, doctors recommend following simple rules. The first and most important thing is to minimize contact of the skin (with an increased number of moles) and ultraviolet radiation. Contact with chemical components should also be avoided. It is not recommended to eat foods that contain food additives that increase the risk of cancer.
It is important to monitor the formation of new nevi, as well as the condition of old ones. Doctors agree that a person needs to be examined by a dermatologist every year in order to promptly identify the development of pathology. It is also necessary to avoid injury to moles, be it mechanical or chemical damage.
Peeling and other dangerous signs of mole degeneration
Experts identify a number of signs that indicate the possible degeneration of a nevus and the development of melanoma.
Such symptoms are considered a reason to visit an oncologist. Any mole that has undergone changes must be removed. Peeling is not the only unfavorable sign. As a rule, there are several more points that will accompany peeling when the nevus degenerates.
- Cracks, crusts and ulcers on the surface of the neoplasm.
- Shiny, smooth surface of the mole, disappearance of grooves.
- Hair loss.
- Change in color of nevus. The color may become uneven and patches of black, blue, purple, red, and white may appear.
- Feeling of fullness, itching, pain in the area of the pigmented neoplasm.
- The appearance of a hyperemic rim around the nevus.
- Increase in size 2 times in 6 months.
- Diameter more than 6 mm.
- The boundaries become fuzzy, merging with the skin.
If there are signs of a change in the appearance of a mole over time, you should see a doctor immediately. A benign neoplasm does not grow and does not undergo transformations, so any, even the most minor, changes in the area of the nevus must be diagnosed by a doctor.
Why are flaky moles dangerous?
Any changes in moles should alert you: they may indicate the onset of malignant degeneration of the nevus. A consultation with an oncologist or oncodermatologist is required if the formation begins to peel off, itch, and then accompanying symptoms are added:
- the mole has changed in size, quickly grown or decreased;
- a flat mole suddenly became convex;
- the edges of the nevus have become uneven and asymmetrical;
- the light mole has darkened;
- after peeling, the formation peels off and falls off;
- hair fell out of the mole;
- nevus bleeds;
- There is pain in the area of the mole and discomfort is felt.
Note! If at least one of the above symptoms is added to the peeling of a mole, you should immediately consult a doctor!
What to do if a mole peels off
photo of a mole peeling off
If signs of changes in the surface of the birthmark are detected - peeling, ulceration, bleeding - you should contact an oncologist who specializes in skin pathology. You should not self-medicate and use products to relieve peeling (scrubs, medicated ointments).
The doctor will conduct a thorough diagnosis of the tumor using a dermatoscope and, if deemed necessary, perform a biopsy. Given the high incidence of melanoma even in young people, most often a mole that has begun to peel off is removed. Then it is examined by histologists and the nature of the process is determined. If the patient comes in at the first signs of nevus degeneration, then the removed neoplasm turns out to be benign in 96% of cases.
When to see a doctor and associated symptoms
Contact a specialist if you notice symptoms of nevus transformation into melanoma. A nevus that can peel off is considered dangerous.
- the appearance of bleeding;
- change of size;
- appearance of a halo;
- swelling, pain on the surface;
- hair loss.
Doctors remove convex formations located on the neck and waist, where mechanical stress occurs.
It is forbidden to remove it yourself; it will lead to the formation of cancer cells. It is not recommended to choose treatment or creams to remove itching on your own.
In patients who come in with peeling moles, benign formations are more often discovered after examination and do not pose any danger. Sometimes malignant growths are discovered and removed.
Treatment methods
photo dermatoscopy of moles
The most popular methods for removing birthmarks and raised moles are the laser method, cryodestruction, electrocoagulation and radio wave method. These methods are used to get rid of elements up to 2 cm in size. Excision with a surgical scalpel is carried out with ambiguous biopsy results and at the discretion of the doctor.
- The laser method is considered the most effective way to get rid of skin tumors. Painful sensations during removal are minimal; local anesthesia can be used by subcutaneous injection of lidocaine. The wound heals quickly - within 2 weeks. Healing takes place under the scab, so it does not have the opportunity to fester. The operation is bloodless.
- The cryodestruction method is inferior in cost to the laser method and does not require such qualified personnel. Liquid nitrogen or dry ice freezes the tissue, which leads to the destruction of the nevus. This method is painful and therefore requires anesthesia. Healing is slower and the likelihood of infection is high.
- Electrocoagulation is a method of using electric current. The operation is bloodless, but quite painful. After removal, a scar remains.
- The radio wave method allows you to get rid of small elements. Removal is almost painless and highly effective. There is no bleeding. This method involves contactless removal of the tumor. The healing process takes 1.5-2 weeks.
Ignoring changes that occur with moles and age spots can have serious consequences. Melanoma is considered the most insidious and malignant tumor, as it metastasizes to internal organs with a tumor thickness of 2 mm. In order to prevent the degeneration of a benign neoplasm, it is necessary to exclude or minimize direct sunlight on moles, maintain proper immune activity and visit a dermatologist 1-2 times a year if there are a large number of moles.
If a mole is covered with a crust, this often indicates the gradual death of its tissues. At first it becomes dark, then rough areas appear on its surface. Subsequently, it completely dries out and disappears.
But another scenario for the development of events is also possible, which is more dangerous, but, alas, no less probable. A crust on a mole may indicate that the neoplasm has degenerated into melanoma, a dangerous malignant tumor of the skin. In some cases you don't have to worry. When is it necessary to see a doctor? It is important to know about this, since skin diseases can sometimes be extremely dangerous.
Treatment of nevus inflammation
Traditional methods
To identify the reason why a mole peels off, a study consisting of 2 stages is used:
- carrying out an external inspection;
- dermatoscopy.
The second method allows you to detect melanoma in the initial stages. After excision of the nevus, the tissue is sent for additional histology examination.
There are several methods for eliminating degenerating formations if the rough mole has not recovered, but has continued to change its structure.
- Laser removal is used for skin spots larger than 2 centimeters in diameter. This is a virtually painless procedure with the option of local anesthesia. The healing period is 14 days.
- Cryodestruction - removal using liquid nitrogen. It is considered a painful procedure. The nevus disappears, but a long healing period is required.
- Electrocoagulation, or exposure to electric current. A rather painful method, after which the formation of scar tissue is observed on the skin.
- Radio wave method - removal without contact and bleeding during the operation process. The healing period is from 9 to 14 days.
- Surgical removal.
Severely dry or rough moles that have begun to degenerate are a dangerous sign of the onset of cancer. Human skin is penetrated by a network of blood vessels, and the penetration of metastases into the blood often leads to the formation of foci of disease in other systems and organs.
The degeneration of a mole in an adult, child or teenager can be stopped by removing a section of skin.
Why children and teenagers are at greater risk:
- a small child is not able to take care of his health on his own, this means that examination and determination of changes must be under the control of parents;
- a child’s skin is very delicate, it is less protected from exposure to external factors;
- most nevi appear in childhood;
- During adolescence, a complex restructuring of the hormonal balance occurs in the body, which is responsible for all processes, including those occurring in the nevus.
Children and adolescents should be aware that moles should be treated with care, and if there is an unusual change in the appearance of the skin, their parents should be informed.
Peeling of a nevus does not always, but quite often signals the beginning of the degeneration of a mole. Melanomas are malignant neoplasms that can be treated in the early stages of the disease. But they can cause significant problems if the symptoms are ignored and the process is neglected, and also contribute to the spread of metastases throughout the body.
Pigmented nevi - moles - benign skin formations. They do not pose a health threat unless they are a nuisance. When a mole begins to peel off, change color, itch, or grow rapidly, this is a reason to consult a specialist, since these may be symptoms of a dangerous pathology.
Diagnostic measures for scaly nevi are carried out by a dermatologist:
- survey, visual inspection of the mole. The specialist collects anamnesis and asks questions about changes in education;
- dermatoscopy, necessary for diagnosing the degeneration of a mole at an early stage. Performed using a device with tenfold magnification;
- histology for the presence of inflammation and malignant cells. It is carried out after removal of questionable and dangerous nevi.
Attention! Histological analysis is a mandatory procedure for an excised mole. If the doctor does not intend to carry it out, the patient must insist on this diagnosis himself.
After removing a mole, an open wound remains in its place. The doctor who performed the operation should give recommendations on how to handle it to avoid infection.
Until a crust forms, the wound should be treated with chlorhexidine or 3% hydrogen peroxide. It is recommended to lubricate the resulting scab and the skin around it with external anti-scar products - Contractubex, Mederma, Dermatix.
Dryness, roughness, peeling and soreness of a mole may be symptoms of its malignant degeneration. Under no circumstances should you delay the examination and treatment of such nevi - melanoma is curable only at the initial stage.
Birthmarks are formations of a benign nature, which generally do not interfere with human life. But there are a number of situations when moles turn from harmless growths into preconditions for a serious condition, degenerating into melanoma (a cancer-type tumor). A sign of unfavorable complications may be a situation where the mole peels off, roughness, and dryness are felt in the area of melanin accumulation.
If the growth dries out and undergoes changes, this is a reason to think about its elimination.
Medicine offers methods for excision of birthmarks:
- destruction by liquid nitrogen;
- electrical coagulation;
- radio wave excision;
- laser removal;
- surgical intervention.
These tactics are relevant when getting rid of elements that have reached a size of 2 cm or more. Excision using a surgical scalpel is carried out in cases where the biopsy shows ambiguous results. Laser technology is relevant when tumors occur. It does not cause pain, does not last long, and the resulting wound heals quickly.
Thus, a flaky mole is a sign of complications that requires immediate consultation with a doctor for diagnosis and therapy.
Related posts:
- Japanese anti-wrinkle creams reviews
- Effective anti-cellulite cream
- Egg white for face against acne
- Effective exercises for back folds
- Japanese massage for face lift Asahi
- Effective masks for deep wrinkles at home
Safe reasons for the formation of a crust on a mole
Let us immediately note that there is no such thing as a mole in dermatology. This is the “folk” name for a benign neoplasm, which in dermatology is called a nevus. The reason for the formation of a crust on a mole can be completely harmless. But only if:
- The growth is small in size. Such nevi are considered absolutely safe in dermatology. And even if a crust appears on such a mole, but no alarming symptoms are observed, then you can turn a blind eye to this little nuisance.
- The nevus is symmetrical and has no “threads” or spots around it. This is a very good sign, confirming the fact that the neoplasm is benign.
- The growth does not cause any discomfort, does not hurt or itch. Under such circumstances, peeling of the skin around the mole may be due to friction of the new growth on clothing.
Note. Despite the fact that the above signs confirm that the growth is benign, it still needs to be shown to a doctor. Especially if a black crust appears on the mole for no apparent reason.
Why does a nevus turn black?
What does it mean if a mole has crusted over? A similar symptom may occur due to the gradual drying and death of the nevus. How does this process happen?
To begin with, the mole flakes off, but does not itch. It may darken or retain its normal shade. No foci of inflammation are observed either in it or in the surrounding tissues. There is no itching, burning, or discomfort.
After the formation of a dry crust on the mole, any processes in its tissues may stop. That is, for a long period it can remain dried out, but be present on the skin.
After a certain time, a person may notice that the crust has peeled off the mole, and it itself has begun to gradually decrease. It may also lag behind the general layer of the skin. You cannot touch such a growth - this process will eventually end with complete drying out and the disappearance of the new growth.
Another reason why a mole has dried out and crusted over may lie in the person’s prolonged exposure to UV rays. In this case, the liquid from the surface of the growth rapidly evaporates, therefore, it becomes dry. But we note that this is by no means a harmless process, since under the influence of ultraviolet radiation, even benign and small nevi can degenerate into a malignant skin tumor.
Important! If a mole dries and peels, then under no circumstances should you tear it off! Even if you see that it will soon disappear, there is no point in speeding up this process. Otherwise, a large wound may form in its place, bleeding may occur, and in the worst circumstances, a malignant tumor may form.
Treatment of moles
After removing an open wound remains in its place . The doctor who performed the operation should give recommendations on how to handle it to avoid infection.
Until a crust forms, the wound should be treated with chlorhexidine or 3% hydrogen peroxide. It is recommended to lubricate the resulting scab and the skin around it with external anti-scar products - Contractubex, Mederma, Dermatix.
Dryness, roughness, peeling and soreness of a mole may be symptoms of its malignant degeneration. Under no circumstances should you delay the examination and treatment of such nevi - melanoma is curable only at the initial stage .
When should you be concerned?
The mole has crusted over, itches and hurts - what could this mean? If you notice such symptoms, you should immediately make an appointment with a dermatologist or dermatologist-oncologist.
A mole that has become crusty and itchy requires special attention. This process may indicate:
- The inflammatory process occurring in the tissues of the nevus. It is indicated by symptoms in the form of itching, redness, and an increase in size of the tumor. In some patients whose mole has darkened and crusted over, droplets of liquid or blood appear on its surface. Such wounds do not bode well. They become easily infected, which can result in the formation of an abscess on the surface of the growth.
- Degeneration (malignancy) of a nevus into a malignant skin neoplasm – melanoma. If a mole peels off and grows, then this process absolutely cannot be ignored. The degeneration of the growth is accompanied by the appearance of “spider-like threads” surrounding it. They can also “spread” in different directions, forming a kind of cobweb pattern. At the same time, the nevus loses its symmetry, becomes uneven, and acquires torn edges.
If a mole is cracked, inflamed and painful, then you should not self-medicate. The only thing that is allowed to be done at home is to treat it with Chlorhexidine or hydrogen peroxide. These are antiseptic agents that will prevent infection of the tumor.
It is also allowed to use decoctions of medicinal plants that have anti-inflammatory, soothing and disinfecting properties. These are chamomile, sage, eucalyptus, calendula.
Note. Such home procedures are allowed to be carried out for a day, maximum two. After this, you must definitely visit a doctor’s office, since traditional medicine relieves symptoms, but does not eliminate the problem as such.
What can a doctor do?
To begin with, the dermatologist collects a detailed medical history based on the patient’s complaints. After this, the growth must be examined, a visual assessment of its condition and examination for the presence of suspicious inclusions is carried out.
But this is not enough. If, based on some signs, the doctor determines that the nevus is of poor quality, or notices that its degeneration is possible, he is obliged to send the patient to the laboratory for a biopsy. This procedure gives the most accurate results, since the selected tissue sample is studied in detail and thoroughly to identify atypical cells.
If the diagnosis of melanoma is not confirmed, but the mole still looks inflamed and causes discomfort, the doctor may prescribe anti-inflammatory drugs. If necessary, antibacterial and wound-healing ointments can be used.
If the presence of a malignant tumor is confirmed, it is urgently removed surgically. After the operation, the patient is registered with an oncodermatologist, and he must undergo preventive examinations every 6 to 12 months, since this disease can recur.
Finally, we note that even if a mole has crusted over and fallen off, you should not pin your hopes on the fact that all the dangers are behind you. Atypical cells can be present not only in its tissues, but also in surrounding ones, therefore, after the disappearance of the nevus, a preventive consultation with a dermatologist is still required.
Diagnostics
Diagnostic measures for scaly nevi are carried out by a dermatologist:
- survey, visual inspection of the mole . The specialist collects anamnesis and asks questions about changes in education;
- dermatoscopy , necessary for diagnosing the degeneration of a mole at an early stage. Performed using a device with tenfold magnification;
- histology for the presence of inflammation and malignant cells. It is carried out after removal of questionable and dangerous nevi.
Attention! Histological analysis is a mandatory procedure for an excised mole. If the doctor does not intend to carry it out, the patient must insist on this diagnosis himself.