Sometimes the appearance of a pimple is not particularly disturbing, but it can not only increase in size, but also acquire a purple tint. Often there are a lot of pimples, and they even start to break out.
Photo 1 - Furuncle on the leg
Furunculosis is a rather dangerous disease that occurs at any age for a number of reasons.

Photo 2 - Furunculosis
For example:
- decreased general immunity;

Photo 3 - Reduced immunity - the presence of staphylococci or streptococci;

Photo 4 - Staphylococcus bacteria - dirt ingress;
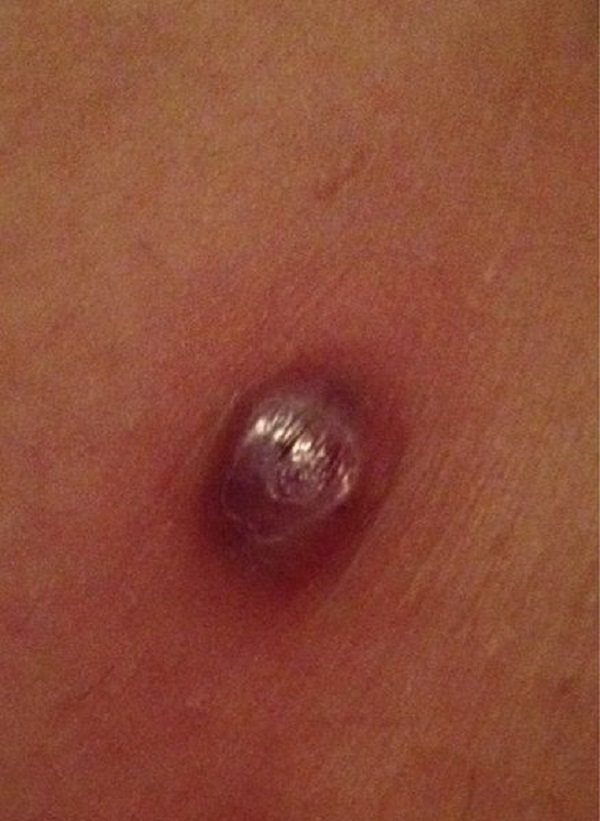
Photo 5 - Dirt got into the wound - inflammation of the hair canal and its blockage in hot weather;

Photo 6 - Blockage of hair canals - anemia;

Photo 7 - Anemia is the cause of boils - getting Staphylococcus aureus into the wound;
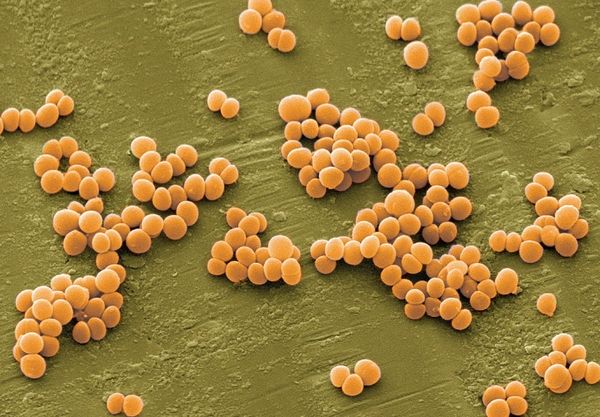
Photo 8 - Staphylococcus bacteria got into the wound - alcoholism;

Photo 9 - Boils can be caused by alcoholism - metabolic disease;

Photo 10 - Poor metabolism - taking hormones;

Photo 11 - Hormones - poor nutrition;

Photo 12 - Poor diet causes boils - hypothermia;

Photo 13 - Hypothermia causes boils - diabetes mellitus and other reasons.

Photo 14 - Diabetes mellitus cause of boil
Since boils like to be localized on the neck, legs, arms, in places where the limbs are flexed, with increased hair growth and friction, attention is paid to them almost immediately.

Photo 15 - Boil on the neck
Features of the pathology
Subcutaneous inflammation, affecting not only the surface of the epidermis, but also adipose tissue, as well as the deep layers of the dermis, can be diagnosed as an internal boil. The damaging element of this disease is the activation of staphylococcal microorganisms that can quickly multiply in favorable conditions.
Manifestations
The symptoms of this disease are usually quite pronounced:

the formation is dense and has a large penetration depth;- severe redness of the inflammation area affects a large volume of tissue;
- headache;
- increased body temperature;
- the patient feels pain when performing any actions in muscle tissue associated with suppuration;
- prolonged formation of a purulent head or its complete absence.
Most often, subcutaneous formations occur on the face and neck, in areas where the sebaceous glands are located and in places of increased sweating: above the lip, in the nose, in the area of the external auditory canal. There are frequent cases of localization of boils on the forearms, thighs and buttocks.
Development of education
The progression of pathology and maturation of the subcutaneous abscess takes several stages:
- Formation of infiltrate. At this stage, bacterial damage to the hair follicle occurs and the formation of an infiltrate that can reach up to 4 cm in diameter. In the area where a group of staphylococci accumulates, redness, swelling and painful tingling are observed.

A purulent-necrotic lesion appears after a few days in the core of the infiltrate and is a small yellowish rod. After spontaneous emptying of the purulent masses, the swelling gradually subsides and the patient’s condition returns to normal.- Regression and healing. The surface, freed from purulent discharge and necrotic accumulations, gradually tightens. However, if the depth of the lesion was too great, a noticeable scar may form on the skin.
Any boil goes through these stages, but the danger of an internal abscess is the too slow formation of a purulent core (in some cases it may be completely absent or grow inward), which significantly slows down the healing process and complicates treatment.
If the treatment is carried out correctly, the formation of boils under the skin should fade away. In cases of complications, the pathology can progress to the stage of recurrent or chronic furunculosis. This condition entails numerous complications: the development of tissue abscesses, meningitis, even sepsis.
Why does an abscess occur?
An internal boil occurs due to an imbalance of microorganisms populating the surface layer of the epidermis. Staphylococcal strains are able to remain on the surface of the skin in a latent state, settling on the mucous membranes.
However, there are factors that can trigger the progression of inflammation:
- severe hypothermia or overheating of the body;
- increased sweating of the skin;

avitaminosis;- dysfunction of various functional systems of the body;
- improper or insufficient hygiene;
- excessive physical activity;
- prolonged emotional stress;
- primary infectious lesions of the body (bronchitis, pyelonephritis, otitis media, sinusitis, tonsillitis);
- long-term use of drugs that suppress the immune system (for cancer);
- frequent trauma to the skin (shaving, insect bites, scratches, scratching for eczema, scabies);
- chronic stages of metabolic disorders (anemia, diabetes).
Dermatologists call the most common reason for the progression of the bacterial environment to be a decrease in the normal functioning of the immune system. Also among the most common cases of boils are a decrease in the protective mechanisms of the skin, its systematic injury and contamination.
In addition, you should know that staphylococcal infection can be easily transmitted in household conditions, so you should use
personal hygiene products.
Pain in the knee joint during flexion and extension: a complete list of causes, how to treat the disease
Have you been trying to heal your JOINTS for many years?
Head of the Institute for Joint Treatment: “You will be amazed at how easy it is to heal your joints by taking every day...
Read more "
Every second person experiences pain in the knees. Pain in the knee when straightening after a long stay in one position is not yet a reason to panic. But constantly recurring pain indicates the presence of changes in the knee joint and requires consultation with a doctor.
The knee joint is the most used joint in the body and is constantly exposed to stress. Many muscles are involved in bending the knee, and when their work weakens, there is an increased load on the joint and its membranes. Discomfort and pain in the knee joint are a manifestation of reversible or other processes that can only be identified by a specialist.
Causes of knee pain during flexion and extension
There are many factors that cause pain when bending, so it is important to undergo a full examination to identify the underlying cause, make a diagnosis and prescribe a course of treatment. In case of a complicated condition, all procedures are performed in a hospital setting. The causes of disturbances may be local changes and disturbances in the functioning of the whole organism.
Local reasons:
- Sprains and tears of the ligaments of the joint capsule of the knee.
- Knee injuries.
- Bursitis of the knee joint.
- Traumatic injuries of the meniscus.
- Bone fractures and condition after fracture of adjacent bones.
- Dislocation and habitual subluxation in the knee joint.
Common diseases that cause pain:
- arthrosis;
- polyarthritis;
- gout;
- arthritis;
- diseases in the lumbar spine;
- infectious diseases;
- purulent process in the joint;
- diseases of the endocrine system;
- osteoporosis.
Find out what causes knee bruises from a fall and how to treat the injured joint.
Causes not related to disease:
- Difficult working conditions.
- Playing sports with uneven loads.
- Excess weight.
- Pregnancy.
Another reason is oncological diseases, the detection and treatment of which occurs only in a hospital setting and under the supervision of the attending physician.
Symptoms of changes in the knee joint
- When bending the knee, a feeling of discomfort or pain occurs, accompanied by a characteristic crunching sound.
- Aching or cutting sensations in the knee joint.
- Increase in local temperature.
- Persistent pain after physical activity.
- Pain in the knee when straightening after sleep.
- Going up or down stairs causes pain in the knee joints.
- Swelling of the joint and changes in the skin are symptoms of an infectious inflammatory process or degenerative changes in the articular surfaces and cartilage tissue. There may be an accumulation of fluid in the joint capsule.
- Crunching in the knee when bending and limited movement when walking. Paroxysmal painful spasms lasting from several minutes to several hours.
- Throbbing pain and muscle cramps that occur after a slight load on the knee joints, for example, when kneeling for a few minutes or during a short walk.
Diagnostics
Treatment of the knee begins only after the patient has undergone a complete examination. Identifying the direct and indirect causes that cause pain when bending the leg will become the basis for a correct diagnosis.
The examination is carried out using the following methods:
- Examination by doctors of several specialties.
- X-ray types of examination.
- Ultrasound.
- Laboratory types of research.
- CT scan.
- MRI.
Find out the main causes of knee pain on the inside, behind the knee and on the outside on the side and how to treat them.
The same banned issue for which Ernst fired Malakhov!
Joints and cartilage will be cured in 14 days with the help of ordinary...
Treatment and rehabilitation measures
The treatment is complex: treating the cause of the disease, reducing symptoms and restoring cartilage in the joint.
For local injuries of the knee joint that cause pain when bending, anti-inflammatory drugs, ointment dressings and compresses are prescribed. Then physical therapy and physiotherapeutic procedures are added. The prognosis is favorable.
Treatment of more complex changes in the knee requires a broader range of drug therapy. For this purpose, the following groups of drugs are prescribed:
- Antibacterial drugs.
- Anti-inflammatory drugs.
- Preparations that restore tissue trophism.
- Medicines that normalize blood circulation.
- Vitamin complexes.
Depending on the severity of the disease, treatment can take place in a hospital or clinic. All physical stress on the knee joint is excluded. Medicines are prescribed in the form of tablets or injections. Before use, an allergic reaction test is always carried out.
You can relieve pain when bending with the help of specific ointments and compresses. Ointments are selected symptomatically. Compresses are made for no more than two hours (as they cool, they are removed earlier). Wearing a special knee brace or applying an elastic bandage is only recommended by a doctor.
Basic drug treatment is supported by the appointment of physiotherapeutic procedures, therapeutic exercises and massage.
Physiotherapy procedures:
- UHF.
- Electrophoresis with drugs.
- Warming up with paraffin.
- Mud treatment.
- Herbal baths.
- Magnetotherapy.
Therapeutic gymnastics is carried out under the guidance of a specialist. For home use only after appropriate training and instruction. There should be no acute pain in the joint after physiological procedures or therapeutic exercises. If pain occurs, physical therapy is stopped. Treatment is adjusted and continued only after the permission of the attending physician.
For all types of pathologies of the knee joints that cause pain during flexion and extension, a salt-free diet is prescribed. Preference in food is given to fruits and fresh vegetables. The cooking process should be steamed or in the oven. You can have boiled foods without spicy seasonings.
Folk remedies for treating knee joints
Herbal preparations will help treat inflammatory processes in the knees. For example, herbal teas are good for relieving inflammation and swelling:
- drink a decoction of flax seeds three times every day. This will improve metabolism and trophism of inflamed tissues in the joint. It is prepared like this: pour two tablespoons of flax seeds into 300 ml of hot water, boil for 10 minutes and leave for about an hour. Take the resulting decoction throughout the day;
- juniper berry tea has a mild diuretic effect and a good anti-inflammatory effect;
- decoctions of clover and parsley also have a general strengthening and antitumor effect;
- a drink made from mint herb and birch leaves is useful for any changes in the knee joints. Pour a glass of boiling water into equal parts of 100 g of dry collection and leave in a thermos for one hour. Drink during the day;
- eating pumpkin in any form has a good effect on the general condition, reducing the inflammatory process in the knees;
- carrot juice with lemon and cucumber juices enrich the body with vitamins;
- A cabbage leaf can be applied to a sore knee for any type of illness. The leaf is crushed a little to release the juice and wrapped around the knee. Cover the top with compress paper or polyethylene. If there are no skin lesions or allergic reactions, you can smear a cabbage leaf with honey and apply it to your knee. Cover everything with wool or cotton cloth. Leave for 2 to 4 hours.
A detailed article on how to treat knee joints with folk remedies.
Preventive actions
First of all, the load on the knee joints is limited, and bed rest is recommended. If you experience severe pain in the knee joint and adjacent muscles when flexing and extending, you should consult a doctor and undergo an examination. It is necessary to balance the diet, limit the content of salt and foods that retain fluid in the body. Vegetable and fruit juices will help establish water-salt metabolism in the body and fill all organs and systems with vitamins.
A timely treatment and preventive course will help avoid serious complications:
- Suppuration in the knee joint.
- Surgical interventions.
- Destruction of cartilage tissue.
- Degenerative changes in bone tissue.
Preventive examination and consultation are required if:
- constant pain;
- discomfort in the knee joints;
- frequent relapses of chronic knee diseases.
In addition, important for prevention:
- Changing working conditions and rational distribution of loads when playing sports.
- Wearing special fixing bandages and bandages for the knee.
- Fight against bad habits (long stay on bent knees, crossed legs).
Taking care of your knee joints is the key to normal functioning of the lower extremities and good health. Healthy knees and legs will help you go a long way in life.
IT IS IMPORTANT TO KNOW! The only remedy for treating joints recommended by doctors! Read more…
Lipoma
The appearance of a small lump on the back, left or right side of the neck due to a lipoma is the least terrible reason why such a phenomenon can occur. In other words, a lipoma is a wen. It is a compacted formation of excess fatty tissue deposits under the skin. When you feel the lipoma, there is no pain, the seal is soft and can move under the pressure of your fingers. It should be noted that such a lump on the neck can remain unchanged for years, but one day it begins to grow rapidly, causing discomfort and inconvenience. A lipoma can only be removed surgically in a clinic.
Atheroma
Such a compacted formation on the left or right is more dangerous, unlike the previous type. Atheroma is a cyst that forms as a result of the sebaceous glands becoming dirty and clogged. Fat microelements and epithelial cells are gradually deposited in this cyst. Atheroma is considered a more dangerous neoplasm. Most often, atheroma occurs near the hairline and is fixed near the diseased gland. Outwardly, it will resemble a lipoma, however, it will be less mobile with a black dot in the center. Atheroma is characterized by a tendency to fester. In such a situation, such a lump grows quickly, is accompanied by pain and eventually comes to the top with pus. It should be remembered here that during surgery it is very important to remove the cyst capsule in order to exclude the possibility of the disease progressing again.
Fibroma
This cone has a compacted round shape with clearly defined contours. At the same time, the color of the skin on the fibroma does not change, and pain is not felt. The formation is benign and often occurs due to genetic predisposition. However, there are cases when fibroma occurs after injuries and inflammatory processes. The formation grows very slowly and there are rare cases when it becomes malignant from a benign form. Such a lump can only be removed surgically, and it will not take much time.
Neurogenic tumors
This tumor usually appears on the right or left side of the neck from the spine. There is no pain in this case. Most often it is a consequence of a neurogenic tumor. A neurogenic cone is characterized as a type of cyst that occurs on the borderline trunk of a nerve or its branch. The main reason for the appearance of this type of lump can be various injuries. Very often lumps such as neuromas and neurofibromas appear on the neck.
Furuncle
This formation occurs due to poor hygiene, a weakened immune system, and also due to hypothermia. A boil is characterized by purulent inflammation of the hair follicle when bacteria enter damaged areas of the skin. In this situation, the lump is not noticeable at first, but the area is very painful and itchy. After a few days, the area swells and a hard core forms in its center. Treatment of a boil occurs exclusively surgically, and constant monitoring of the wound is necessary. Do not self-medicate under any circumstances, as this can lead to blood poisoning, which can transfer the affected cells to the brain. In such a situation, the consequences are sad for life.
Enlarged lymph nodes
This is the most common reason for the formation of bumps. It is quite easy to identify them. A newly formed lump on the neck on the right or left, not far from the ear under the lower jaw, will be a lymph node that is inflamed. Here it must be said that such a lump is inactive, very dense and hurts when pressure is applied to it. Accompanied by fever, headache and general weakness of the body. Basically, enlarged lymph nodes are observed with a weak immune system or as a complication after an infectious disease. However, remember that if the lump is not accompanied by pain, this may be a sign of a malignant tumor, such as lymphogranulomatosis or lymphocytic leukemia.
Be very attentive to where the lump appears and what symptoms accompany it. It is very important to correctly determine the type and cause of the appearance in order to choose the right treatment.
How to get rid of boils?
Diagnosing the disease and identifying the degree of penetration of the pathological process is possible only at an appointment with a qualified specialist. An internal boil, or abscess, in most cases can be eliminated using conservative therapy. Surgical opening of the boil is resorted to only in cases of complicated forms of pathology, if the abscess progresses, growing inside the tissues. In this case, the boil is opened under anesthesia, the wound is treated and a sterile bandage is applied.
Conservative treatment methods
In the infiltration stage, treatment is carried out using the following methods:

application of dry heat to the area of large inflammation;- use of tightening ointments (Ichthyol ointment, Levomekol, Gepar-sulfur)
- laser therapy;
- UHF therapy;
- antibiotic therapy (in cases of complicated internal furunculosis): Tetracycline, Amoxiclav.
If the process of suppuration has taken a severe form and is accompanied by general intoxication of the body and severe tissue swelling, the patient requires urgent hospitalization and surgical intervention. Typically, the doctor applies a sterile cloth soaked in a weak solution of salicylic acid to the affected area, which corrodes the epidermis and allows purulent masses to come out of the tissue.
Opening a boil on your own can lead to blood poisoning, so doctors usually do not recommend home treatment.
However, it is possible to somewhat alleviate the symptoms of the disease at the initial stage and accelerate the formation of a purulent core, which means the breakthrough of the boil:
- relieving itching and discomfort using antiseptic solutions (camphor, salicylic) and iodine tincture;
- applying applications with an antibacterial anti-inflammatory agent (Ichthyol ointment);
- wet warm compresses to relieve pain (bergamot oil, chamomile).
You should know that frequent water treatments and visits to the bathhouse when the boil is maturing are prohibited.
How to treat
There are several ways to cure a boil on your leg at home. All of them require contacting a dermatologist to prescribe appropriate treatment.
Primary treatment for boils consists of treating the inflamed area of skin with antiseptic agents. The use of such products as hydrogen peroxide, brilliant green, salicylic alcohol, methylene blue, etc. is allowed.

The damaged area must first be prepared - long hair (for men) is shortened with scissors (shaving is prohibited - the consequence will be further infection of the body) and lubricated with antiseptics at least 2 times a day.
Treatment for a boil on the leg depends on:
- on the characteristics of the inflammatory process (with or without complications);
- on the general condition of the patient (fever, malaise, presence of additional diseases, pregnancy);
- from the presence or absence of other boils on the body (this is important, since there is a risk that it will be necessary to treat not individual boils, but systemic furunculosis).
You can cure a boil on the leg, which only makes itself felt by a thickening formed under the skin and mild pain, using 2% salicylic acid or 70% ethyl alcohol. Solutions are used several times a day to treat the inflamed area on the leg in order to resolve the boil.
It is necessary to treat a boil on the leg when a purulent-necrotic core has already formed inside it (this can be seen from the purulent point located in the middle of the boil) only with the use of anti-inflammatory external agents.
Drugs
Treatment of a boil on the leg is carried out by lubricating it with a 5% iodine solution. In case of severe pain, the boil is injected with novocaine as an anesthetic and lincomycin, an antibiotic to which staphylococci are sensitive (other drugs can be used).
At home, experts recommend smearing the surface of boils treated in this way with a solution of fucorcin. After this, a dry bactericidal dressing is applied to the boil.
For boils on the leg, treatment is aimed at accelerating the maturation of subcutaneous inflammation. If you detect the problem in a timely manner and begin treatment before pus begins to accumulate inside the boil, you can get rid of the pimple in a short time.
To do this, use a solution of iodine, boric acid or alcohol. Antiseptic treatment is carried out three times a day until the tumor completely disappears.
If a boil appears on the leg, it must be treated. It doesn't go away on its own. There are different methods for treating abscesses. If the suppuration is single, then treatment at home is possible, but if the patient’s health condition rapidly deteriorates, then it is better to consult a specialist.
The appearance of a boil on the leg should not go unnoticed by the sick person. If not treated correctly, an infectious skin disease can lead to infection of the entire body.
Treatment of boils can be divided into three stages.
At the first manifestations
The hair around the infectious area is carefully trimmed, the swelling is lubricated with iodine and brilliant green at least twice a day.
If the infectious focus progresses (2-3 days)

The affected area is treated with salicylic alcohol (2% - percentage);
Vishnevsky ointment, Konkov ointment, ichthyol are used. A thick layer of the drug is applied to the affected area and bandaged with a sterile gauze bandage.
If your general condition worsens, you should consult a doctor. He will prescribe treatment with antibacterial drugs based on novocaine. The choice of antibiotics depends on the causative agent of the infection.
The group of penicillin antibiotics (Amoxicillin, Amoxiclav, Ampicillin) is currently considered not the most effective way to treat a group of coccal microorganisms.
Antibiotics of the cephalosporin group (Cefazolin, Cefotaxime) are more effective than penicillins. The advantages of these antibiotics are ease of use (powders and injections) and low cost.
Gentamicin is considered effective in treating boils on the leg. But it has a number of contraindications (pregnancy, childhood, kidney disease, liver disease, gastrointestinal tract).
Levomecithin in the form of an ointment is often prescribed by doctors for its ease of use.
When ripe and opened
This can happen on its own or with the intervention of a surgeon. The root of the infectious focus must come out, otherwise the boil will continue to break out. The painful wound is treated with antiseptics (hydrogen peroxide or miramistin) and a sterile bandage is applied.
The most common method of treating this disease is drug therapy. Today, there are a significant number of such drugs that demonstrate good effectiveness in the fight against dangerous infections.
READ MORE: Boil on the labia, female organs, boil on the organ
It goes without saying that there are folk remedies that are used to combat boils on the lower extremities. Their effectiveness has traditionally been a subject of debate among medical representatives, however, judging by reviews, their use helps get rid of boils without any consequences.
Naturally, this applies to cases when purulent inflammation occurs without exacerbations and is in the early or middle stages of development.
At the moment, the following folk recipes are the most popular:
- lotions with calendula. A decoction of ordinary calendula is prepared, the collection of which can be purchased at any nearest pharmacy. Next, you need to moisten a cotton pad or a piece of clean gauze in the prepared product and apply it to the affected area. The top of the lotion is covered with a tight and clean bandage;
- coltsfoot - fresh leaves of this plant must be crushed until they begin to release juice. After this, they are applied to the boil for several hours;
- flatbread made from eggs and honey. One of the most effective folk remedies. The flatbread is prepared as follows: one egg yolk is mixed with one teaspoon of natural honey. Rye flour is added to the resulting mixture. After this, the dough is kneaded, from which a thick cake is formed. It should be applied to the boil for about 10 hours, for example, at night, carefully securing it with a gauze bandage;
- gruel of onions and milk - you need to take regular onions and finely grate them. A small amount of milk is added to the resulting slurry, which will help reduce the aggressiveness of the onion. The mixture is applied directly to the site of inflammation for about 12 hours, while being fixed with a bandage.
Treatment of a boil on the leg using traditional methods is a purely individual matter. If a person does not trust traditional medicine, it would be better for him to use the help of traditional medications. In any case, before starting treatment with traditional recipes, you need to consult a doctor who will confirm or deny the possibility of such therapy.
Surgery is the last resort for treating this disease. The surgeon's office is equipped with all the necessary tools and devices, with the help of which such an operation will take place as quickly as possible and with minimal risk of complications.
The method and duration of treatment for boils on the leg is adjusted in accordance with a number of criteria, such as:
- Stage of papule development
- Specifics of the abscess (standard, with complications)
- Number and location of foci of inflammation (multiple rashes are a symptom of systemic furunculosis)
- General condition of the patient (pregnancy, presence of other pathologies)
A medical examination is the most important stage in the treatment of a boil on the leg. Only a specialist is able to adequately assess the complexity of the pathology, establish the causes of its manifestation and give recommendations for effective control of abscess symptoms at home.
Medicines
Medical practice includes an extensive arsenal of tools for treating boils on the skin of the feet:
- Immunomodulators and vitamins
- Antibiotics (used to treat severe forms of the disease)
- Analgesics
- Anti-inflammatory drugs
- Antiseptic drugs
Immediately after the boil appears, it should be treated around it with alcohol, after removing hair from the affected area. Next, the abscess itself is lubricated with a solution of iodine or brilliant green.
Fucorcin has an antibacterial effect, and ichthyol ointment also helps to ripen the rod and release the purulent contents. At the first symptoms, Vishnevsky ointment is used, which also helps to draw out pus.
Antibacterial drugs are prescribed in the form of injections or tablets. Experts recommend taking cephalexin, metronidazole and others.
If the seal is very painful and cannot break through, an incision is made during the operation, treating the inflamed area with anesthetics. Stitches are applied if necessary.
READ MORE: Legs hurt after dexamethasone
After the incision, a wound remains that must be carefully treated with antiseptics. To do this, apply compresses with ointment, for example, tetracycline or gentamicin, to prevent re-infection.
Traditional medicine is aimed at eliminating the inflammatory process and speeding up the release of purulent contents. Most often, various herbal decoctions and infusions are used, as well as lotions made from them.
Before home treatment, it is better to consult a doctor and choose the most effective methods of folk or traditional treatment. Usually, to treat a boil on the leg, it is enough to disinfect the tubercle and apply a bandage with a special ointment or a mixture of natural components of traditional medicine.
What is and features of internal furunculosis
The source of inflammation is bacterial microorganisms - staphylococci, which actively multiply in a favorable environment.
Externally, the internal appearance of a boil (boil) resembles a lump. Most often it is red. The formation is quite hard and may look like a subcutaneous ball.
This type of formation occurs in most cases:
- in the armpits:
- on the head, under the hairline;
- on the neck;
- on the eye;
- in the groin area (folds);
- inner thigh;
- gluteal region;
- lower back;
- earlobes;
- shin area.
Under unfavorable circumstances, this phenomenon poses a threat to the health and life of the patient.
Treatment for finger abscess
If a toe or hand breaks out near the nail, treatment may vary depending on the degree of development of the disease.
For mild inflammation, warm baths with anti-inflammatory substances or a compress for swelling and inflammation can help. These are more of a first aid measure, but they can contribute to recovery in the early stages of paronychia development.

narwhal toe near the nail photo
In more advanced cases, you need to consult a doctor (make an appointment with a doctor online). Moderate paronychia can be cured without surgery using antibiotics. You may be prescribed dicloxacillin, clindamycin, or cephalexin.
If it comes to severe suppuration, you cannot do without surgical intervention. Complications of paronychia can lead to severe inflammation of the phalanx, loss of the nail, and blood poisoning.
The essence of surgical treatment is an incision in the area of the nail fold. Then the pus is removed through this channel, and the wound is disinfected. It is possible to combine the previously described methods, for example, additional antibiotics.
If the abscess on your finger has been present for a long time, it is likely that the nerve endings have been damaged. This can be determined by the painful color of the skin or by testing the sensitivity of the area with a sharp probe (ordinary needle). In such cases, the operation proceeds without the use of anesthesia.
Symptoms and causes
The appearance of an internal boil is sudden. A person notices the formation of a hard ball that does not move, but rises above the skin layer. The boil is developing quickly. It begins to swell and may turn red. In a few days its size can reach the size of a cherry. Touching the source of inflammation is quite painful. Severe acute pain is also caused by simple mechanical movements associated with the work of the muscles closest to the boil.
In most cases, a white dot is observed in the center of the formation - a passage that acts as the core of an inflamed abscess. After the abscess begins to mature, purulent masses will erupt through this passage. Sometimes subcutaneous occurs without exit. This is dangerous; a mature formation can “burst” inward, spreading the infection into the blood and organs.
Common causes of internal furunculosis:
- frequent mechanical damage to the skin;
- lack of hygiene:
- wearing tight synthetic underwear and clothing;
- using contaminated items (shaving blades, earrings, towels);
- swimming in dirty ponds;
- nervous tension, stress;
- problems with the functioning of the immune system;
- hormonal changes in the body;
- long-term use of medications that inhibit natural defenses;
- avitaminosis;
- unbalanced diet;
- regular consumption of alcoholic beverages;
- chronic skin diseases;
- metabolic disorder;
- frequent hypothermia or exposure to high temperatures;
- hepatitis, tuberculosis, bronchitis.
Isolated cases of furunculosis are more often associated with personal hygiene problems. But frequent and multiple formation of subcutaneous ulcers may indicate existing problems in the body or the development of diseases. To determine why a boil has formed under the skin, you need to seek help from a specialist.
Features of a child
A boil in a child resembles a tumor in appearance, which is filled with purulent masses. The reasons for the formation of boils on the legs are no different from adults. A poorly treated abrasion on the knee often provokes the formation of boils. When abscesses appear constantly, seek help from a pediatrician or dermatologist for advice. It may be necessary to undergo additional tests to identify the root cause of furunculosis.
If the resulting boil on a child’s leg is small, then in order to cure it, warm compresses are applied to the affected area until it ripens. Compresses must be made carefully so as not to disrupt the integrity of the surface vesicle and not provoke a breakthrough ahead of time. Treatment at home is possible after consultation with a doctor. Show an abscess that does not go away within 10 days to a dermatologist.
Features
It is quite difficult for a person without special education to distinguish a chiry from a regular subcutaneous pimple. There are characteristic distinctive signs of an internal boil.
| Characteristics | Furuncle | Acne |
| Size | Large, sometimes up to several centimeters in diameter | No more than a pea |
| Appearance | Red, brown. Smooth glossy surface. | Red White. A bulge under the skin. |
| Soreness | Pain occurs with and without touching. Refers to the muscles. | Painful - pain is felt only when touched. |
| Localization | Groin area, buttocks, armpits, back, head. | Any part of the body. Mainly on the face - chin, cheeks, forehead. |
| Maturation process | Up to 10 days. Accompanied by acute pain. | 3-4 days. Painless |
| Purulent discharge | Copious, with blood. | Slight, no impurities. |
| Associated symptoms | Local hyperthermia, possibly a general increase in temperature. | Asymptomatic |
| Purulent head | It is weakly expressed, sometimes there is a boil without a head. | Vividly expressed. |
| Possible traces | Scars, keloids. | Pigment spots. |
Pubic boils most often occur on the inner thigh, in the crease between the leg and the pubic area. May have an elongated shape. Easily injured by underwear, abrasions and wounds appear on the surface of the bump. Causes discomfort when walking.
On the scalp, the formation of boils is noticed mainly at the back, closer to the neck. Reaches large sizes. The appearance causes particular discomfort; a person can only lie on his side, without moving his head.
If a person suspects the formation of a boil, he should consult a doctor. If necessary, surgical opening of the abscess is performed.
How to treat bursitis of the knee joint?
In the treatment of infectious diseases, the following types of treatment have proven themselves to be effective:
- At the initial stage, the patient needs to keep rest, which is supplemented with cold compresses and compressive bandages.
- Anti-inflammatory drugs are prescribed: ibuprofen, surgam, ketoprofen, etc.
- Aspiration of synovial fluid. The decision to perform it is made if there is a large volume of fluid in the bursa. After anesthesia, antiseptic treatment of the inner surface of the synovial bursa is carried out.
- Corticosteroid injections. The most commonly taken drugs are hydrocortisone and diprospan, which help relieve acute pain.
- Muscle relaxants. Help eliminate muscle and vascular spasms.
For the treatment of bursitis that is infectious in nature, the following drugs and treatment methods are indicated:
- Antibacterial therapy. Antibiotics prescribed by a doctor are taken orally or as intramuscular injections.
- Non-steroidal anti-inflammatory drugs. Designed to remove the manifestation of pain. Alternatively, corticosteroid injections may be used.
- Cleaning the bursa from purulent contents through surgery or drainage of the joint capsule.
In the case when the inflammation process has become severe, as well as in the presence of adhesions in the synovial bursa, the doctor may begin to treat bursitis of the knee joint using bursectomy. We are talking about surgical removal of the synovial bursa.
Bursitis of the knee joint can also be successfully treated with topical medications. We are talking about the use of ointments and creams with NSAIDs. In addition to them, the use of special compresses with dimexide, dressings with Vishnevsky ointment, Capsaderm ointment, etc. is indicated for treatment.
Stages of development of a subcutaneous boil
The average duration of furunculosis is 10 days. During this time, education goes through 3 stages of its development:
- Infiltration. There are signs of tissue infiltration - swelling, redness. A thickening occurs under the skin. The person feels constant tingling and itching at the affected area. A distinctive feature of a boil is the growth of infiltration around the hair. This is due to the spread of staphylococci in the follicle cavity. This stage is considered as the maturation of the abscess.
- Purulent necrotic. Approximately 4 days after inflammation, a white head appears in the center of the compaction, which is a purulent core. The abscess protrudes above the surface of the boil. The tissue around him is red and hot. Over time, the skin on the surface core becomes thinner, the contents come out in the form of purulent masses mixed with blood. The symptoms of the malaise weaken, the person feels obvious relief.
- Healing. As soon as the formation breaks through, a furunculosis crater appears in place of the previous compaction - a hole in which pus was located. Wound healing takes several weeks (sometimes a month). The affected area dries out. A thin crust forms, under which new healthy skin grows. If the growth is small, there will be no marks left on the skin. Large ulcers, located deeply, leave behind keloids or scars.
Regardless of what stage subcutaneous furunculosis is at, a person needs to remember precautions. It is unacceptable to open the seal at home. Hygiene supplies must be exclusively individual. It is better to avoid touching the affected area whenever possible.
Symptoms
The development, or maturation, of the boil occurs in stages.
First, a small itchy red spot appears on the leg. A slight tingling sensation may be felt. After a short time, a small compaction-nodule forms under the skin, which can be felt with your fingers. The skin in this area swells. A tubercle appears (look at the photo).
After a few days, an infiltrate forms in the center of the tubercle - this is an accumulation of pus (dead leukocytes) interspersed with blood. Necrosis of nearby tissues occurs, which spreads inward - a purulent boil core is formed, going quite deep.
A small yellow head of this rod is visible at the top of the tubercle. This stage is accompanied by increased pain and swelling.
The boil can reach a diameter of up to the size of a walnut (3-4 cm). A ripening boil is shown in the photo.
If the process proceeds normally, then the intervention of a surgeon is not required; everything happens at home. After a week, the boil fully matures and bursts out. Pus comes out of it. An ulcer remains in place of the boil, which heals to form a white scar. In the photo you can see the mark left after the boil.
A furuncle on the leg, as well as similar formations, with any other localization, for example on a finger, back or in the nose, develops according to a standard pattern, going through the stages of infiltration, necrotization and healing. At each stage, appropriate treatment is necessary.
Infiltration
The formation of boils begins with the appearance of a subcutaneous reddish lump on the leg. Purulent necrosis is concentrated in its center - the core; the deeper it is, the larger the area the pathological process covers.
Gradually, the pimple takes a conical shape, the color of its surface varies from white-green to blue-violet. With proper treatment, after 3-5 days the boil matures and opens without outside help. Along with the purulent masses, dead tissue is rejected, leaving an ulcerative cavity in its place.
READ MORE: Fungus on your feet? Athlete's foot - Everyone is at risk! What is foot fungus
Treatment methods for neoplasms
In most cases, treatment of boils is conservative. The patient is prescribed a course of antibiotics (Tetracycline, Amoxiclav) if the disease is severe and accompanied by severe symptoms of malaise. In moderate conditions, laser and ultraviolet heating is used to treat abscesses, and “dry heat” is used. During the period of infiltration, it is important to use ointments that can draw out pus - Vishnevsky, Levomekol Ichthyolova, Gepar sulfur. Sometimes compresses with salicylic acid are used to speed up the release of purulent masses. The substance corrodes the upper layer of the epidermis, allowing pus to come out. Performing such manipulation at home is strictly prohibited.
In severe cases, when there is a risk of internal effusion of the abscess contents, surgical intervention is performed. The tissue is cut and the contents of the boil are removed. The resulting crater is treated with antiseptic solutions. If necessary, a special device is introduced - drainage - to release the accumulating exudate. After 5 days, the drainage is disposed of.
Traditional medicine suggests accelerating the ripening process of chiryak with the help of a baked onion head, which is applied to the inflammation. A decoction of chamomile or bergamot, aloe or Kalanchoe leaves, heated alcohol or honey-wheat cakes are used.
Treatment Options
Doctors do not recommend treating chiri until it matures. All you need to do is speed up the ripening process. For this purpose, warming compresses and dry heat are used. When the boil on the leg is large, the maturation process is accelerated by UHF heating. After opening the abscess, antiseptic solutions are poured into the cavity to avoid complications. The affected surface of the leg is treated with antibacterial drugs and wound healing agents.
Be sure to make sure that the rod comes out, otherwise repeated suppuration is possible.
If ulcers on the legs appear constantly and take a long time to heal, in parallel with treatment, measures are taken to increase immunity. Systemic antibiotics are prescribed for extensive furunculosis or for the recurrent nature of the pathology. Along with antibiotics, live bacteria must be taken to restore the intestinal microflora.
Treatment with medications at home
- Vishnevsky ointment is an anti-inflammatory and wound-healing agent. The ointment draws out pus and speeds up healing time. It is used during the ripening process and after opening the chiria. The leg needs to be smeared every day at night until it heals.
- "Levomekol" and "Levomethyl" are antibacterial drugs. Apply as soon as the leg is swollen and until complete recovery. The use of ointment excludes the addition of bacterial complications after opening the chiria.
- “Syntomycin liniment” is a local antibiotic that disrupts the protein synthesis of pathogenic microorganisms. It has an anti-inflammatory effect, and due to the novocaine content, the ointment anesthetizes the area affected by the boil.
- “Ichthyol ointment” is an affordable remedy that helps remove boils on the legs and other areas. Effectively removes purulent mass from mature chiria and accelerates scarring.
- "Chlorhexedine", "Hexoral" and "Hexicon" are antiseptic solutions used to rinse the cavity after the necrotic plug has come out.
How to treat with folk remedies?
- A mixture of Vishnevsky liniment and fir oil. A teaspoon of each ingredient is mixed, the resulting mixture is applied to the chiri, covered with a piece of cotton cloth and secured with a roll plaster.
- Flatbread made from honey, eggs and rye flour. The ingredients are mixed until thick enough to form. The resulting cake is applied to chiri for 12 hours.
- Baked onion. The onions baked in the oven sprinkled with flour are fixed on the chiriye for 8-10 hours. The product is capable of resolving the infiltrate.
- Horseradish leaves. The ground leaves are applied as a compress to the boil and left for 5-6 hours.
- Traditional medicine recommends brewing and drinking herbal decoctions of yarrow, chamomile, thyme, mint, eucalyptus leaves and elecampane root to increase immunity in case of furunculosis.
Possible complications
Despite the relative “simplicity” of the disease, the complications of boils are quite serious. More often they arise due to attempts to independently open a subcutaneous (internal) boil or as a result of involuntary mechanical damage.
Depending on the location of the formations, complicated processes are distinguished between local, distant and general. The first include: erysipelas, carbuncles, phlegmon, abscesses. The second ones are phlebitis, lymphangitis, lymphadenitis. The latter carry the risk of meningitis, organ abscesses and blood poisoning.
To prevent the development of complications, which, in most cases, are difficult to treat, you need to go to the doctor at the first signs of illness. The sooner the doctor assesses the patient’s condition, the more effective subsequent therapy will be. The basic rule for a person with a boil is that there is no attempt to squeeze, scratch or puncture the boil.
A subcutaneous boil is an unpleasant and painful phenomenon. In order not to encounter it, it is better to follow preventive measures - monitor hygiene, use individual items, strengthen the immune system.
In addition to the sole, a boil on the leg can appear anywhere - on the toes (on top), on the skin of the lower leg, under the knee, on the thigh and in the groin area. A single boil does not cause much trouble and goes away on its own in about a week. But there are situations when boils “walk” along the leg, moving from zone to zone or immediately appear in large numbers (furunculosis).
A boil on the leg can appear in both a child and an adult. The most unpleasant thing is when it occurs during a “separation” from civilization, for example during a long hike. It is there that the most favorable conditions for a boil are created - lack of conditions for proper hygiene, increased sweating, abrasions due to long walking and uncomfortable clothes or shoes.
This is what a boil on the leg looks like in the photo.
Why is boil dangerous for children?
In most cases, single boils are not dangerous , but when identifying them, it is extremely important to follow one simple rule: unlike a regular pimple, squeezing a boil is strictly prohibited. Reckless actions to independently open the pathology are fraught with sepsis, infection, phlegmon, thrombophlebitis and chronic furunculosis.
READ ALSO: What should I bathe my child in if he has allergies or skin rashes?
If furunculosis develops against a background of weakened immunity, several lumps may form simultaneously. In this case, the young patient risks experiencing severe swelling, redness of the skin, high fever and headaches.
Causes of a boil on the leg
The immediate cause of a boil on the leg is Staphylococcus aureus, which lives on the skin and mucous membranes of the nasopharynx in almost all people. It belongs to the group of opportunistic flora. This means that it can acquire pathogenic, disease-causing properties when certain conditions occur. The most important conditions:
- the presence of a minimal defect on the skin (abrasion, wound, abrasion, scratch);
- constant skin irritation from chemicals;
- increased activity of sweat glands and increased skin hydration.
- An additional risk factor is a violation of the defense system - immunity. The following lead to decreased immunity:
- poor nutrition, excess carbohydrates and excessive passion for fast food;
- lack of intake of B vitamins and antioxidants;
- lack of trace elements and minerals, especially iron;
- chronic fatigue syndrome;
- chronic stress;
- gastrointestinal problems and dysbiosis, chronic infectious diseases;
- concomitant skin diseases;
- taking medications from the groups of cytostatics, immunosuppressants, antibiotics, glucocorticoids;
- hormonal imbalance.
- Sometimes the appearance of furunculosis indicates the presence of another serious pathology:
- diabetes;
- rheumatoid diseases;
- HIV - infection;
- metabolic disorders.
Tight, uncomfortable shoes contribute to the appearance of boils in the foot area. In the groin area, a boil is provoked by underwear that does not fit, especially from synthetic fabrics. Compliance with personal hygiene rules plays an important role. Don't discount leg shaving and hair removal.
Pathogen and causes of the disease
Bacteria of aureus, less often white, staphylococcus have the opportunity not only to penetrate into the cavity of the follicle, but also to develop rapid vital activity there due to a decrease in the activity of the immune response. The insidiousness of the microbe, which is responsible for the appearance of a boil on the leg, lies in the fact that staphylococcus bacteria are always present in small quantities on human skin. The vast majority of these are conditionally pathogenic strains, which the immune system does not allow to activate their vital functions.
And under favorable conditions, staphylococcus quickly develops vigorous activity, first penetrating the hair follicles, and then, with inadequate treatment or no treatment at all, spreading through the bloodstream to other organs.
The reasons for the appearance of a purulent-necrotic boil of the outer covering can be both exogenous and endogenous. Any factor that adversely affects the activity of the immune system can provoke purulent-necrotic inflammation. Therefore, a boil on a leg or finger appears more often in the autumn-winter period, when the risk of hypothermia increases and the frequency of colds rises.
Exogenous (external) provocateurs of a boil are:
- Scratches, cuts, abrasions of the skin;
- Frequent leg injuries;
- Constant contamination with chemical compounds or organic dust from coal, cement or lime;
- Scratching after insect bites;
- Systematic failure to comply with personal hygiene rules.
Endogenous (internal) factors contributing to the formation of a boil are:
- Poor nutrition, exhaustion;
- Anemia;
- Obesity;
- Increased sweating;
- Nervous tension or stress;
- Endocrine diseases;
- Diseases of the digestive system;
- Vascular pathologies;
- Alcohol intoxication.
Symptoms of a boil on the leg
A single boil on the leg does not cause much discomfort. The first signs of its appearance are a burning sensation, slight itching and redness on the skin. The diameter of the redness usually does not exceed 5 mm. The inflammatory process in the hair follicle develops, involving the sebaceous gland and the muscle that lifts the hair. This is accompanied by pain in the area of inflammation. If the abscess is in the groin, then the pain is quite sensitive. Boils on the toes are painful.
During the development process, a purulent core is formed in the center of the boil, represented by dead microbes and blood cells (leukocytes). After spontaneous removal of the rod, the pain decreases, the wound usually closes without scar formation.
Diagnosis is not difficult. Once you see a photo of furunculosis on your leg, you can easily recognize it in reality.
A complication occurs in the form of a carbuncle. Many boils merge into a single abscess, reaching 10 cm in diameter. Symptoms become general:
- temperature;
- chills;
- headache;
- malaise, weakness;
- deterioration of health;
- enlargement of regional lymph nodes;
- severe pain in the affected area.
This pathology is much more serious and treatment of a complicated boil on the leg at home is unacceptable.
Although the localization of boils on the leg of a child or adult is observed less frequently than others, neglect of the question of how and when to treat it leads to vascular complications. Developed arteritis or thrombophlebitis causes severe pain in the leg and is fraught with fatal complications.
Children have another unfavorable feature. Due to the immaturity of the immune system, in case of poor nutrition and proper care in dysfunctional families, skin phlegmon and sepsis quickly develop, from which the child dies.
If a boil has formed on the thigh
When a boil appears on the thigh, you must immediately treat it with an antiseptic and apply an insulating bandage. This is especially important when a boil appears on the inside of the leg, in order to eliminate friction.

Photo 31 - Boil on the thigh
Inflammation can occur due to infection or sweat getting into the hair follicle, and it is also often a harbinger of diabetes mellitus if the boils are in the groin. Poor personal hygiene, excessive sweating and excess weight can also lead to inflammation. When a boil appears on the side of the thigh, you can use folk remedies.

Photo 32 - There are many reasons for the appearance of a boil on the thigh
Typically suggested for use:
- attach an aloe leaf;
- use bandages with silver applied to them;
- can be cauterized with iodine;
- honey and flour cakes;
- calendula flower ointment;
- compress with honey, salt and egg yolks, flour.
However, if the boil is large in size, the so-called carbuncle, then it is better to resort to surgery and open this boil in a hospital setting. When inflammation occurs inside the thigh, it especially causes a lot of trouble.

Photo 33 - Carbuncle on the leg
The temperature may rise, local inflammation and tissue compaction may occur, which can be treated with ointment, antibacterial agents and physical therapy. Therefore, the doctor will tell you what to treat here, because a boil can cause quite a lot of trouble if it is left unchecked.

Photo 34 - The doctor will select an effective treatment
Inflammation on the inner side of the thigh interferes with movement, so after removing the abscess the doctor may give you a sick leave for several days.

Photo 35 - Boil on the inner thigh
Stages of ripening of a boil on the leg
As in any other place, a boil on the leg has general stages of ripening. In typical cases, the following is observed:
- infiltration stage - redness, thickening, formation of a papule, painful even on palpation;
- necrotic stage - the formation of a purulent-necrotic rod, which looks like a yellowish or dark dot in the center of the hyperemic area;
- spontaneous rupture of the abscess and release of the rod with pus and a small amount of blood;
- healing of the wound.
The total duration of the process in an uncomplicated course does not exceed 10 days.
What does it look like in the photo?
Look at the examples of boils in the photo.
READ ALSO: Atheroma and lipoma: what is the difference and what are the differences?
Treatment of a boil on the leg
On the one hand, the simplicity of the problem, on the other, deadly complications. So how to treat a boil on the leg?
First rule. Although the leg, unlike the back, is a very accessible area, squeezing out an abscess, even with a formed rod, or unauthorized opening of an abscess using improvised means is unacceptable.
How to treat a single boil on the leg in the absence of general symptoms at home? As easy as pie. At the infiltration stage, it is sufficient to treat the area of redness with an antiseptic solution with cleanly washed hands and apply an aseptic bandage. You can apply a bandage with Levomekol. The purpose of this stage is to prevent generalization of inflammation. After the rod comes out, wound healing agents are appropriate. The slightest deviation from the standard course or lack of effect within 2 days requires a visit to the doctor.
Treatment of a boil on the leg with folk remedies
Traditional medicine offers recipes on how to treat a boil on the leg at home. They can be used for isolated occasional boils; all other cases are treated by a surgeon. Treatment of a boil on the leg prescribed by a doctor can be performed at home. Traditional medicine offers:
- onion - fry 1 white slice in a frying pan without water, oil and salt, cool slightly, apply to the boil, secure with a bandage;
- salt, bread crumb and grated onion are used to form a flat cake, which is placed on the leg;
- honey, egg, rye flour - make a flatbread;
- Mix 50 grams of grated laundry soap with 50 grams of grated beeswax, 50 grams of bread, 1 tablespoon of honey per 180 ml of water, cook over low heat, and after cooling, form a flat cake.
Treatment of a boil on the leg at home is shown in the photo.
It is undesirable to use folk remedies for people from risk groups with concomitant diseases or reduced immunity. It is safer for them to immediately seek help from a surgeon.
A boil on a child’s leg should be treated as the doctor says, not a traditional healer.
Treatment of a boil on the leg with medications
Permissible only as prescribed by a doctor. It is carried out both at home and in a hospital. The doctor chooses treatment tactics depending on each individual case. In some cases, surgical treatment is performed, including opening the abscess, removing the purulent-necrotic core, drainage and bandage with medication.
Antibacterial therapy is carried out by oral administration of anti-staphylococcal or broad-spectrum antibiotics. Subsequently, daily dressings and physical therapy are prescribed. In the chronic form, acupuncture is effective.
To strengthen the immune system, a course of autohemotherapy, injections of vitamins, and immunocorrectors are carried out.
As for the use of ointments for boils on the leg, we can name the most popular and proven:
- Vishnevsky ointment;
- ichthyol ointment;
- Levomekol;
- Solcoseryl accelerates healing).
When did a boil appear on the knee?
If you suddenly have a boil on your knee, you should pay attention to it. When bending your leg, the boil may burst, so try to limit movement and apply a bandage.

Photo 36 - Boil on the knee
Since the slightest inflammation on the knee causes pain, you can take painkillers, use antimicrobial ointment and attend UHF procedures. The main thing is to avoid friction on clothing and dirt getting into the wound. To do this, you will have to apply bandages and use plasters.

Photo 37 - Rest the knee
A daily shower is required, as well as treatment with antiseptics until the rod appears.

Photo 38 - Be sure to shower daily
Attention! If there is severe inflammation and redness of the surrounding tissues, you should immediately consult a doctor to remove the contents of the boil and subsequent treatment.
When localized under the knee, everything is a little simpler. There are no hair follicles there, and therefore not a boil, but another formation will develop there. The same applies to formations on the foot, toe and heel.

Photo 39 - Inflammation under the knee
Prevention of this disease:
- maintaining hygiene;
- improvement of immunity;
- weight loss and blood sugar control;
- wearing loose cotton clothing in hot weather;
- treatment of chronic diseases;
- treatment of inflammation sites with camphor and salicylic alcohol;
- taking vitamins or yeast.
It is also necessary to find out the cause of frequent furunculosis. This can be done by a doctor by ordering an examination of the patient. After which a comprehensive treatment is selected, not only locally, but also generally to improve the patient’s health.
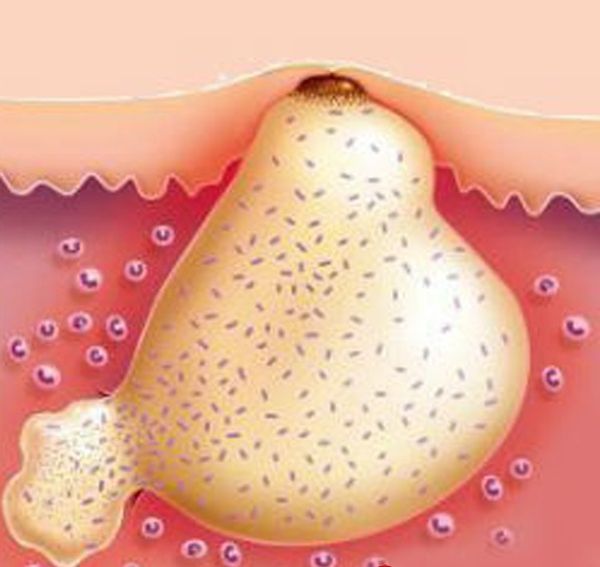
Photo 40 - The boil needs to be treated comprehensively
Prevention of furunculosis on the leg
In addition to general recommendations on proper nutrition, a healthy lifestyle, maintaining hygiene measures, wearing clothes and shoes of the correct size, you can additionally recommend vaccination with staphylococcal toxoid in case of chronic furunculosis.
Carry out hair removal in compliance with the requirements of asepsis and antiseptics in trusted beauty centers. Pay special attention to your pediatrician's recommendations for feeding and caring for your child.
You will receive the most competent treatment aimed at preventing relapses of furunculosis and secondary prevention from a specialist - a purulent surgeon.
Causes of the disease
Like many other diseases, boils appear against a background of decreased immunity. Healthy people living an active life have a lower risk of developing boils than sick people and those who regularly drink strong drinks and smoke. The strain can remain on the human body for a long time, inactive, until an opportune moment arises. Without knowing the reasons why a chiryak forms on the leg, it is difficult to hope for a long-term effect of treatment.
The following factors are related to the formation of a favorable environment for the life of bacteria:
- Lack of hygiene. Staphylococci multiply more happily on a dirty body. The use of other people's towels, clothes and poor-quality hygiene products also plays a role.
- Skin damage. Bacteria penetrate into the body through microcracks, small scratches, and abrasions. One of the most important rules of prevention states that after an injury occurs, the patient must immediately disinfect the injury and cover it with a plaster or bandage.
- Weakening of the immune system. Immunity suffers due to lack of vitamins (poor nutrition or terrible diet), stress and chronic diseases.
- Diabetes mellitus and various malfunctions of the body often lead to the appearance of boils.
If a boil is not treated promptly, it can develop into a serious health problem. There is a high chance of chronic furunculosis and the formation of boils on other parts of the body in large numbers. Chronic furunculosis is very difficult to cure, if possible.

With sufficient hygiene, the risk of developing a boil is reduced
How is the disease diagnosed?
In order to identify foot skin fungus, it is enough to simply examine the epidermis of the feet, nail plates and interdigital parts. Typical signs help confirm the presence of the disease. To find out which fungus is the causative agent, a scraping is taken from the affected nail plate.
This scraping is sent to the laboratory for analysis. Bacteriological culture helps to very accurately identify the irritant. Typically, such results are ready within a week after the test. Once the results are received, the doctor will be able to tell you how to cure the fungus.
Treatment for fungus on the toes can only begin after an accurate diagnosis has been made. Only your doctor can tell you how to get rid of the fungus. It is important to remember that the cure must be comprehensive. It could be:
Whatever the reason, the doctor will tell you how to treat it after examination. You should not resort to self-medication.
Local treatment of the disease
Local therapy is effective in the first stage of the disease, when the infection affects the dermis between the fingers. Local medications are actively used for parallel nail damage.
Only a dermatologist can prescribe a suitable remedy. Self-medication is contraindicated, since the drugs have a lot of side effects. This can cause great harm to health.
When the folds between the fingers become infected, it is recommended to use creams and ointments. The dermis in this part is very delicate, so any careless actions can easily injure it. This will cause the infection to spread.
Apply a thin layer of product over cracks. When treating the dermis, you should apply the medicine not only to the infected areas, but also 2-3 cm around. This will help get rid of fungal elements on healthy dermis.
In what form to buy the drugs depends on what the fungus looks like. For husking and dryness, it is recommended to purchase ointment. She penetrates deep inside. Effective in the fight against fungus that has become chronic. The ointment is always applied under the bandage. In this case, the active components penetrate even deeper.
If the infection worsens, creams should be used. This form is quickly absorbed into the epidermis. Medicines in the form of creams do not penetrate into the deeper layers.
Some drugs are produced in two forms at once. In this case, experts recommend applying the ointment at night and using the cream during the day. The choice of drug depends on the type of pathogen.
Curing a fungal infection is possible not only with local remedies, but also with tablets. A systemic approach is indicated for extensive infection and when the fungus spreads to the nails and feet. The most commonly prescribed drugs are those based on fluconazole and itraconazole. To relieve itching and inflammation, the following is prescribed:
Such medications very often cause third-party reactions. These include:
Long-term use of such drugs can become the root cause of a malfunction of the entire body. For this reason, funds can only be taken after a full examination by a specialist.
The course of therapy with antibacterial medications must be completed. Otherwise, there will be no effect from the funds taken. Achieving a cure will be extremely difficult.
Treatment with folk remedies
Treatment with folk recipes involves the use of a variety of means: baths, ointments, creams, decoctions, solutions, compresses. This method of treatment is effective as part of complex therapy for the disease. The most effective recipes are:
For successful treatment, it is recommended to combine local therapy with systemic therapy. Folk remedies are prescribed as additional drugs. The choice of agents depends on the stage of the disease and the presence of a secondary infection.