Dysplastic nevus occurs in every twentieth person on the planet. It has no age or gender restrictions. Most often, the pathology manifests itself in the form of a spot larger than 6 mm. There are several types of such neoplasms; they have different shades and clinical forms. The condition of moles should always be monitored to avoid adverse health consequences.
Classification of nevi
There can be a lot of birthmarks; they differ from each other in their structure and type of formation.
What types of moles are there? First of all, these are congenital and acquired pigmented spots on the skin. Congenital appear immediately after birth and are caused by malformations of the skin, acquired - appear over time, by 2 years of life, during puberty and are benign tumors of the skin. Nevi also differ regarding the place of their formation in skin cells:
- Lentigo or borderline. These are pigment spots formed between the dermis and epidermis;
- Dermal. These are raised nevi that appear in the dermis. Most often these are flesh-colored or light brown spots;
- Epidermal. These are pigmented neoplasms in the upper layers of the skin;
- Complex or combined. These are spots, often convex, of a mixed type, which form both in the deeper and on the surface layers of the skin.
It is impossible not to note the following classification of nevi:
- non-hazardous formations, i.e. neoplasms that cannot develop into a malignant tumor;
- melanoma-hazardous, i.e. nevi in which the risk of degeneration is very high or the process of malignancy has already begun;
- atypical moles, i.e. having suspicious symptoms of degeneration, but not yet becoming dangerous, can remain on the skin all their lives and not cause cancer.
An important classification is this type of mole:
- Vascular formations. These are pinkish, red and bluish-red spots on the body. The shade depends on the vessel from which the nevus is based. They can be cavernous and capillary, some of which are convex and angular, while others are flat;
- Not vascular nevi. These are pigmented growths on the skin. They can have different colors and shades, convex and flat, large and small, hairy or without hair.
A hemangioma mole is often found in children, but what is it? Essentially, this is a type of vascular neoplasm on the body that appears in the first days of a baby’s life. They can be either small or gigantic in size. The danger of such birthmarks is the risk of thrombus formation, which leads to deterioration of blood clotting. Up to 8 months, such a neoplasm can actively grow; up to a year and a half, growth can stop. By the age of 5, self-removal of hemangioma is often observed, i.e. there is a chance that it will disappear on its own without special treatment.
Etiology of the disease
It is impossible to determine exactly what exactly provokes the formation of dysplastic nevi on the skin, and what factors contribute to the migration of melanocytes and their concentration in one local area. There are several assumptions about the etiology of the disease:
- Nevi are a consequence of exposure of human skin to large amounts of direct sunlight.
- The tendency to form a dysplastic nevus is inherited.
- The presence of human papillomavirus in the blood contributes to the formation of such skin tumors.
- Low immunity can cause the appearance of a large number of moles.
- Autoimmune diseases that occur in a latent form for a long time precede the development of dysplastic nevi.
- Pregnancy and any hormonal changes in the body contribute to the active growth and division of melanocyte cells.
Pregnancy is a possible cause of dysplastic nevus.
It is extremely difficult to identify a nevus prone to malignancy without knowledge and skills. Diagnosis is carried out in a medical institution, and the sooner this is done, the better for the patient.
Congenital melanocytic nevi
What is detoxification of the body
They are found in approximately 1% of newborns, they are divided by size: giant ones have a diameter of more than 20 cm (in adults), small ones - less than 2 cm, the diameter of intermediate ones lies between these indicators. Congenital nevus is characterized by the presence of melanocytic cells in the lower part of the reticular layer of the dermis, between bundles of collagen fibers surrounding skin appendages, nerves and blood vessels. Sometimes these cells spread into the subcutaneous fat. Their histological picture is often unclear. They may have the histological features of a borderline, complex or intradermal nevus. Some moles that arise postnatally exhibit histological features of congenital ones. Moreover, congenital nevi are not always easy to differentiate from other pigmented formations based on the clinical picture, although parents indicate that the mole was present at birth. Differential diagnoses include Mongolian spots, café au lait spots, smooth muscle hamartoma, and dermal melanocytoses (nevi of Ota and Ito).
Small congenital moles are localized on the lower part of the body, in the lumbar region, on the shoulders, chest, and in the proximal extremities. These nevi can be flat, raised above the skin, warty or nodular. Their coloring in varying proportions includes brown, blue or black. Due to the difficulties of clearly identifying small congenital nevi, data on the frequency of their malignant transformation are contradictory. According to anamnestic criteria, approximately 15% of melanomas are formed from small congenital pigmented formations. According to histological criteria, elements of a congenital nevus in melanoma are found in approximately 3-8% of cases. Removal of all small congenital nevi is not justified, especially in light of the fact that melanomas from congenital nevi occur extremely rarely before puberty. When deciding whether or not to remove a nevus, take into account its localization and the possibility of constant clinical monitoring, the risk of formation of a disfiguring scar, the presence of other risk factors for melanoma and clinical manifestations of atypicality of the nevus.
Have questions or something is unclear? Ask the article editor - .
Giant congenital pigmented nevi occur with a frequency of less than 1 case per 20,000 births. They are localized mainly at the back of the body, but can also be located on the head or limbs. Their particular significance is determined by the fact that they predispose to melanoma and may be accompanied by melanocytosis of the pia mater. The latter most often occurs when the pigmented neoplasm is located on the head or along the midline of the body, especially if it is accompanied by satellite melanocytic nevi. The presence of melanocytes in the pia mater and brain parenchyma leads to increased ICP, hydrocephalus, seizures, mental retardation, movement disorders, and melanoma. The latter can be diagnosed by a thorough cytological examination of the CSF to identify cells containing melanin. Asymptomatic melanosis of the pia mater is detected on MRI in almost 30% of cases of congenital giant nevi. The overall incidence of melanomas in giant congenital nevi is estimated to be approximately 5-10%. About 3% of all melanomas arise from them. 50% of melanomas arising from congenital giant nevi develop by age 5. The mortality rate for them is 45%. There is no consensus regarding the management of congenital giant moles. The decision is made with the participation of a pediatrician, dermatologist, plastic surgery specialist and taking into account the wishes of the parents. If localized on the head or above the spine, MRI is indicated to exclude melanosis of the central nervous system. The presence of the latter makes complete excision of the skin nevus useless. If CNS melanosis has been ruled out, early excision of the mole and closure of the defect by stretching or skin grafting reduces the number of nevus cells and therefore the risk of melanoma, but often at the cost of a disfiguring scar. Even so, nevus cells deep in the subcutaneous tissue elude removal. It is useless to biopsy any mole. It is indicated only when the nevus is enlarged. The frequency of prospective observation in the first 5 years of life is 6 months, then annually. Taking photographs at each examination helps to catch changes.
Treatment
What is RF face lifting
Therapy for single pigment spots involves their radical removal. Multiple dysplastic formations cannot be removed surgically. In such situations, patients are usually prescribed applications of a 5% solution of Fluorouracil, followed by monitoring the condition every six months. In addition to these methods, patients are often prescribed a course of interferon therapy.
Strict adherence to all doctor’s instructions is the main condition for success in the prevention and control of cancer. For this reason, persons with borderline age spots should not self-medicate. Remember, melanoma is one of the most aggressive malignant tumors - today, timely excision of the tumor is the main way to prevent the process of malignancy of atypical nevi.
Surgical removal
Urgent diagnosis and surgery are required in a situation where the syndrome of dysplastic pigment formations shows even minimal dynamics, for example, it itches, bleeds or increases in size. Along with this, experts recommend not waiting for any signs of “revival” of the neoplasm to appear and removing the stain already at the initial stage of formation. The method of surgical removal is selected taking into account the size and shape of the pigment spot.
Thus, for large formations, exclusively the classical method of excision with a scalpel is practiced. Nevi up to 1 cm in size are removed using laser treatment
At the end of this procedure, there are no scars left on the patient’s body, which is extremely important when the pigment spot is located on the face. In addition, small nevi can be removed using:
- Electrocoagulation is a method that allows you to get rid of a mole bloodlessly. The procedure is performed under local anesthesia. The tumor is removed using a metal loop through which current passes. In order to prevent blood loss during electrocoagulation, a small part of healthy tissue is cauterized along with the affected areas, which contributes to the formation of scars.
- Cryodestruction – involves exposing the mole to liquid nitrogen. The procedure lasts only a few minutes and does not cause the patient any negative sensations - there is no need for pain relief.
- Radio knife - this method of removing tumors is considered the most gentle. Under the influence of high-frequency waves, painless excision of tissue occurs, followed by evaporation of atypical cells. The procedure does not require pain relief. The total duration of the manipulation, as a rule, does not exceed 20 minutes.
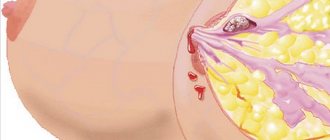
Dysplastic nevus and melanoma.
What is laser septoplasty
Dysplastic nevus is clinically stable in the vast majority of cases. However, there is some evidence that some of these moles develop into skin melanoma. There are a number of studies confirming changes in DNA composition, cytogenetic damage, and the reactivity of atypical melanocytes of dysplastic nevi with monoclonal antibodies directed against various melanoma antigens. The progression of DNA abnormalities leads to melanoma. But, a dysplastic nevus is not an inevitable precursor to melanoma. Currently, the likelihood of melanoma is estimated based on crude indicators such as the total number of moles, the presence and number of clinically atypical dysplastic nevi, along with other factors such as the occurrence of melanoma in the patient himself or his family.
Number None or several (Many (>50) nevi
Size Less than 5mm Varies from small to large, some over 5mm
Coloring Standard, uniform coloring Several or many moles with irregular or random coloring, redness of the skin around
Boundaries Well defined Irregular or indefinable boundaries
Roush et al. and Nordlund et al. Australia More than 5 mm in diameter, irregular borders and variable coloration 34 7 7.7
MacKie et al. Scotland More than 5 mm in diameter and variable color +/- inflammation 38 20 2.1–4.5
Holly et al. USA At least 3 of 6 criteria: indeterminate borders, irregular borders, variable coloration, >5 mm, skin redness, raised skin edges 55 17 3.8–6.3
Halpern et al. USA >4 mm, presence of spot in nevus, variegated color, irregular or indefinable borders 39 7 8.8
Garbe et al. Germany At least 3 of 5 criteria: >5 mm in diameter, non-paved edges, indeterminate edges, color variability, presence of a speck or bump in the nevus 45 5 7
* The relative risk of degeneration of one or two dysplastic nevi is 2.1%; for 3 or more 4.5%
† Relative risk of degeneration from 1 to 5 dysplastic nevi, 3.8%; for 6 or more atypical nevi - 6.3%
Causes
It was noted above that scientists cannot yet say with certainty what provokes the migration of melanocytes.
There are only assumptions that certain situations and circumstances can cause the appearance of a dysplastic nevus. These include:
- Hormonal changes.
- Taking hormonal drugs.
- Pregnancy.
- Infectious diseases.
- Menopause.
- Hereditary predisposition.
- Unfavorable environmental conditions (radiation, toxic substances). Pregnant women are especially sensitive to these factors.
- Visit to the solarium.
- Long sunbathing.
- Inflammatory reactions in skin injuries of various etiologies.
- Weak immunity.
We draw your attention to the fact that dysplastic nevi are not a genetic disease, that is, they are not inherited. However, a person inherits a predisposition to their formation.
Carrying out the operation
The operation can only be performed under local anesthesia, and a scalpel is used for this. Modern laser technologies are not used, just as radio waves are not used, since such technologies may not help, and even harm in this case.
Only with the help of a surgical scalpel is it possible to completely remove affected areas of skin with nevus and melanoma, and the operation is carried out quite quickly.
Not only the affected spot itself must be removed, but also about 3 mm of skin around the spot. This can be explained by the fact that atypical cancer cells are able to spread around the spot exactly to this distance. After the operation, an atraumatic cosmetic suture is applied, which is small in size and heals quickly with proper care.
After surgery, the skin recovers quite quickly, but there is a risk of re-formation of such nevi, and therefore it is very important to monitor one’s own condition throughout a person’s life, and not just during wound healing and the postoperative period
Symptoms of dysplastic nevus
It is quite easy to recognize the dysplastic appearance of a nevus, due to the fact that it has a bright color and asymmetrical shape. It practically does not rise above the surface of the skin and reaches no more than eight millimeters in diameter. Most often, these moles appear on the buttocks, legs, palms and parts of the body covered with hair and on the chest of women.
Clark's nevus does not have a clear outline, but has a small round or oval bulge in the middle. A feature of this formation is the uneven distribution of melanin. The same mole can have different shades of brown and sometimes even red. Upon visual inspection, dots and spots around the source of inflammation are clearly visible on the surface of the formation. An atypical mole is characterized by the appearance of hair on its surface.
You should seek medical help if the following symptoms appear:
- black and thick hairs appeared on the surface of the nevus;
- the mole suddenly changed in size or began to bleed;
- the color of the formation has changed;
- pain, burning and itching appeared;
- the surface of the formation became rough.
It is customary to distinguish three stages of development of dysplastic nevus:
- enlarged melanocytes form formation chains;
- round lesions form from accumulated melanin;
- Bridges appear between foci of inflammation.
Due to the fact that dysplastic nevus is similar to melanoma, it can be difficult to identify a malignant tumor at the initial stage.
Clark's nevus has an uneven shape
What to do if there are dysplastic nevi on the skin?
There is an opinion on the Internet that “all dysplastic nevi should be removed.” I consider this point of view incorrect for the following reasons:
- A very small percentage of nevi that look atypical upon examination turn out to be so upon histological examination.
- An even smaller proportion (0.0001%) of truly dysplastic nevi have a chance of becoming melanoma
- Skin melanoma can develop not from a nevus, but against the background of unchanged skin.
In this regard, for people who have dysplastic nevi, I usually recommend the following:
- Regular self-examination once a month with measurement of existing atypical nevi using a ruler. Optimally – with photographic recording of the result
- Examination by an oncologist once every 6 or 12 months. The frequency depends on the number of nevi.
- It makes sense to remove elements that are difficult to access for self-examination, as well as those that have changed in a short time
- Protect skin from the sun
Therapeutic measures for nevus
Symptoms that require immediate contact with a dermatologist:
- the mole has changed color over a short period of time;
- black, coarse hairs appeared on it;
- the neoplasm burns and itches;
- blood appears on its surface from time to time;
- the nevus has sharply increased in size;
- the surface of the mole became rough, with cracks.
Any slowness can cost the patient his life, so you should contact a derma-oncologist immediately if you detect at least one of the above symptoms.
In most cases, histological studies show the presence of a benign tumor, which is not recommended to be removed. It is recommended to resort to radical methods of treatment, including surgical intervention, when a mole is located on the face, neck, is large in size and bothers the patient as a significant cosmetic defect. A nevus should also be removed when it is located in hard-to-reach places or is constantly in contact with clothing. Mechanical damage is the most common cause of degeneration of nevi into malignant tumors. If there are a large number of neoplasms on the body, then the largest and brightest moles must be removed.
Removing nevi with a scalpel is fraught with the formation of scars, so today there are more and more supporters of other methods of getting rid of the problem. One of these methods is cryodestruction, in which the formation is deadened using liquid nitrogen, and nearby areas of the skin are not affected.
The use of a laser eliminates skin infection; this method is bloodless and allows the patient to quickly return to a normal lifestyle without scars, but there is a possibility of leaving part of the nevus. Another method is electrocoagulation, when an atypical nevus is removed using electric current, but it is only applicable to small formations.
Traditional medicine can reduce the size and intensity of pigmentation of moles, even slow down the process of formation of new ones, but before using any means, you should definitely undergo examinations and use them only under the strict supervision of a doctor.
In this regard, dandelion has proven itself well, the decoction of which is taken orally, and moles are lubricated with milk. A mixture of crushed walnuts and baby cream will help if you have damaged a nevus
You should not ignore celandine, which, when mixed with Vaseline, will prevent the development of skin cancer. They also use pineapple juice, honey, lemon juice, but one should not get carried away with traditional medicine in order to avoid missing the emerging pathological processes
Prevention
It is almost impossible to prevent the appearance of such neoplasms on the skin, since there are a lot of provoking factors that cause the development of dysplastic nevus. However, there are a number of recommendations that will help significantly reduce the likelihood of developing precancerous skin conditions:
- Avoid exposure of the skin to direct sunlight during the hot season, and also do not resort to insolation in solariums.
- Follow the rules of a balanced diet, consuming plenty of vegetables and fruits, as well as lean meats. Refusal of fast food will reduce the content of waste and toxins in the body.
- Constant self-monitoring of the condition of nevi. If there is a suspicion that the tumor is enlarging, crusts, ulcers or other growths appear on it, which, when touched, provoke pain and itching, you should immediately consult a specialist.
- Annual clinical examination, at which, as practice shows, dysplastic nevi are discovered.
It is impossible to completely prevent the development of nevi that are prone to degeneration into cancer. But following simple rules will help you detect the problem in time and decide on the principles for eliminating it. Self-medication should be completely excluded, as in most cases it is ineffective.
Causes of Clark's nevus
Atypical moles are formed due to local movement of pigment cells under the influence of reasons that are not fully understood. The pigment melanin, which is produced by melanocytes located in different layers of the dermis, determines the shade of the skin and is designed to protect it from the harmful effects of insolation (ultraviolet radiation). In this case, the pigment is found in all skin structures in the same amount. But in people with a predisposition during fetal development or immediately after birth, melanocytes filled with melanin migrate to various areas of the skin. Atypical familial birthmarks are formed - small formations that begin to gradually grow during puberty and become clearly visible.
A nevus is a collection of melanocytes overflowing with melanin.
Sporadic (single) nevi occur in a different scenario. Most researchers believe that ultraviolet radiation and the human papillomavirus play a certain role in the mutation and proliferation (accelerated cell division) of pigment cells. The provocateur of the movement and point accumulation of melanocytes is always sharp hormonal changes - the onset of puberty, pregnancy, etc.
It is possible that a significant decrease in the body’s defenses plays some role in the formation of dysplastic nevi, since cases of numerous atypical moles have been reported in connection with skin blistering diseases and some other pathologies that cause immunosuppression (immune suppression).
The risk group for familial dysplastic nevus includes immediate relatives of carriers of atypical moles. It has been proven that the predisposition to the appearance of formations is transmitted in an autosomal dominant manner. Whether a child will develop nevi or not largely depends on the characteristics of his body and the influence of external factors. The closer the relationship with carriers of the pathology, the higher the likelihood of developing multiple nevus syndrome.
The risk of malignancy of Clark's nevus exists due to the persistence of proliferative activity (readiness for increased division) of immature melanocytes in the epidermis and the presence of cell atypia of varying severity.
The danger of Clark's nevus, especially the familial type, is the readiness for malignant transformation into melanoma
Sporadic
They are called acquired precursors of melanoma (skin cancer).
These formations can be single or multiple. The number of spots in a group is not limited.
There are two types of single sporadic dysplastic nevi:
- A – without degeneration into melanoma.
- C – with degeneration into melanoma.
In general, sporadic solitary nevi increase the risk of developing a malignant tumor by 7-70 times.
They are in form:
1. “Fried eggs.” Such a nevus is a flat spot of brown shades with a raised part and can be as follows:
- Very small (from 1 to 15 mm).
- Medium (from 15 to 100 mm).
- Large (from 100 to 200 mm).
- Giant (more than 200 mm).
2. Lentigo. These formations are flat, with a smooth surface. Their color varies from dark brown to black. The sizes are as follows:
- Medium (up to 100 mm).
- Large (over 100 mm).
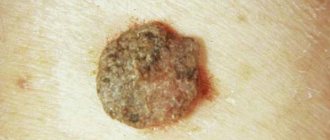
3. Keratolytic dysplastic nevi (pictured below).
Keratolytic nevi have a bumpy, brown surface. In size they are medium (up to 100 mm) and large (over 100 mm).
4. Erythematous. They appear as a pink birthmark. In size, erythematous nevi are large (up to 200 mm) and giant (more than 200 mm).
Classification of nevus removal
Many specialists themselves prescribe getting rid of moles, but only if necessary. Otherwise, such a procedure is a cosmetic operation and not a health improvement for the patient. You should not contact a surgeon if you have performed a self-diagnosis and decided that the nevus is dangerous. Today, there are other examination options to identify the diagnosis:
- dermatoscopy,
- histology.
If histology is the best and most accurate method for determining the diagnosis, then dermatoscopy is an atraumatic method. During histological examination, it is necessary to first completely excise the nevus from the skin and only then can it be checked. Dermatoscopy involves making a fairly accurate diagnosis without removing the nevus. Today there is also digital dermatoscopy, which allows you to create an entire “nevus map” for each patient. This way, changes in nevi will be recorded with precise equipment. It is necessary to undergo examination by a dermatologist or oncologist at least once a year.
If you are prescribed removal of a nevus, then what options are open to you?
- Cryodestruction. This is a method of removing nevus using liquid nitrogen. Unfortunately, it is not always possible to accurately predict the depth of the nevus, so sometimes a repeat procedure may be required. In addition, a thermal burn may appear on the skin, which increases the risk of scar formation and long wound healing;
- Electrocoagulation. In this procedure, an electric current is applied to the skin around the nevus. After this, the pigment formation is removed, and a crust appears on the wound. Due to a thermal burn, the wound may take longer to heal, but the risk of scarring is lower than with cryodestruction;
- Radiosurgery. This is a consequence-free method of removing a nevus using a “radio knife”, i.e. high frequency radio waves. There is no contact with the skin, the method is suitable for removing any nevi;
- Laser surgery. This is a non-contact operation to remove a tumor from the skin using a laser beam. The operation lasts only a couple of minutes, does not require anesthesia and has an excellent aesthetic effect. Ideal for removing age spots from exposed areas of the body;
- Surgical method. This is a classic operation to remove a tumor using a scalpel. An excellent method for excision of a malignant tumor, a large spot. However, this method will leave a scar, but it can be dealt with.
It is difficult to say how to properly remove a mole, because each method has its own advantages. We advise you to talk with Elena Vladimirovna Salyamkina, this surgeon will tell you the best option for your case. In addition, she will be able to perform the operation efficiently and painlessly in the shortest possible time so that you will be satisfied with the results.
Acquired melanocytic nevi
They are accumulations of melanocytic cells formed due to the proliferation of melanocytes at the border of the epidermis and dermis. Their cells are similar in origin to melanocytes, and possibly identical. Less popular, but widespread, is the theory of the dual origin of moles - from superficial cells - melanocyte derivatives (melanocytic nevi) and cells of the deep layers - derivatives of Schwann cells (neuroid nevi).
Epidemiology
During childhood, the number of acquired melanocytic nevi increases gradually, in adolescence - sharply, in young age - more slowly. In the 1st-4th decade of life, their number is at the same level, and at a later age it slowly decreases. On average, an adult has 25-30 melanocytic nevi. The more such formations, the higher the risk of melanoma. In each case, the number of these formations is determined by exposure to sunlight in childhood, especially intermittent ones, the intensity of solar exposure with fair skin, and the tendency to sunburn and freckles rather than an even tan. An increase in the number of these tumors is also accompanied by immunosuppression and chemotherapy.
Symptoms
The course of nevocellular nevi is well known. They are divided into borderline, complex and intradermal. In children, more than 90% of nevocellular nevi are borderline - melanocytes proliferate and form clusters at the border of the epidermis and dermis. Borderline nevi are located on any part of the skin, are relatively small, clearly defined, flat, varied in shape, and have a brown color of varying intensity. They consist of cuboidal or epithelioid pigment cells that form clusters at the border of the epidermis and dermis just above the basement membrane. Sometimes these formations, in particular those located on the palms, soles, and genitals, remain borderline throughout life, but in most cases they become complex: melanocytes migrate into the papillary layer of the dermis and form clusters at the border of the epidermis, dermis, and in the dermis itself . If melanocytes above the basement membrane stop multiplying, then their accumulations remain in the dermis and the mole becomes intradermal. When mature, complex and intradermal nevi protrude above the surface of the skin and acquire a convex shape, the shape of a wart or a pedunculated formation. Slightly protruding moles above the surface of the skin are usually complex, while significantly protruding moles are intradermal. With age, accumulations of melanocytic cells undergo involution and nevi gradually disappear.
Treatment
Acquired pigmented nevi are benign formations. They undergo malignant degeneration very rarely. Alarming symptoms requiring excision and histological examination are the rapid enlargement of a mole, the appearance of uneven coloring with spots of red, brown, gray and black, pigment incontinence, jagged and uneven edges, surface changes - peeling, erosion, ulceration, compaction, the appearance of new moles around existing and enlarged regional lymph nodes. In most cases, they are caused by irritation, inflammation, maturation, and the usual changes in moles in adolescence - darkening, gradual enlargement, elevation above the surface of the skin. When assessing the indications for excision and histological examination, one should take into account Risk factors and the desire of the parents to rid the child of a cosmetic defect. Excision is a safe outpatient operation, which is justified if there is any doubt about the benignity of the formation.
Methods of treating neoplasms
The main method of treating the tumor is surgery, followed by excision of the nevus. The following indications are required to perform the removal procedure:
- the presence of a hereditary factor for the development of melanoma (in close relatives);
- malignancy (degeneration) of the spot into cancer (melanoma).
In the presence of multiple nevus syndrome, the patient must undergo examinations to record the dynamics of tumor growth. It is not recommended to remove all nevi, as there is a significant risk to the patient's health. The examination proceeds as follows:
- constant monitoring of the patient (general health, presence of concomitant pathologies);
- recording the condition of nevi (photography of neoplasms, at least 2 times a year).
All procedures are carried out by a dermatologist; the dynamics of growth and the presence of changes in nevi is recorded by comparing photographs of the previous examination. It is necessary to remove tumors if changes in the nevus are detected:
- visually the growth of the spot increases;
- growth dynamics are unstable, upward;
- the shape of the spot changes;
- the surface of the nevus changes (becomes bumpy, compacted, rough);
- the color of the spot changes (from light to deep dark shades);
- unpleasant sensations (itching) appear.
Surgery
Surgical intervention is carried out when the patient’s health is stable, after a comprehensive examination, in order to detect and eliminate other pathologies that interfere with the operation. The patient's general health may not allow surgical intervention if the nevus degenerates into cancer. In this case, surgery is not performed, but alternative treatment methods are used:
- use of antitumor drugs (cytostatics);
- The use of medications is carried out externally (locally) and internally.
Fluorouracil is used topically, the drug is applied to napkins, and the application is made to the affected areas of the skin.
Surgical treatment, features of its implementation
Removal of nevi has a number of features:
- a scalpel is used to excise tumors;
- the use of laser and radio wave therapy is excluded;
- it is not necessary to use general anesthesia;
- local anesthesia is used;
- the stain is completely removed;
- 4 mm of tissue around the nevus is excised (to prevent cancer cells from entering healthy tissue);
- It is necessary to apply a cosmetic suture at the end of the surgical intervention.
Symptoms
Dysplastic nevi have a heterogeneous shape and unclear boundaries. A bright color is noted, the shade of the formation depends on the number of melanocytes in a particular area of the skin. Initially, nevi appear in small numbers. Their numbers can constantly increase, in some cases the formations cover the entire surface of the skin on a certain part of the body.
Distinctive features of dysplastic nevi:
- The presence of pigmentation from the lightest pink and brown shades to deep black. Usually, within one formation, different shades are observed.
- Elevation of the formation above the skin level.
- A lumpy surface stands out, with an elevation closer to the center.
- Nevi are almost never characterized by an even shape and have asymmetrical, unclear contours.
- Typically, pathologically thick hairs grow from the formation.
- Dysplastic nevi are localized mainly on the arms, upper torso, chest, and head.
The difference between a benign neoplasm and a malignant one
- Signs indicating possible processes of malignancy of a dysplastic nevus:
- Acceleration of growth rates, the diameter of the formation increases by 2 times or more in 1-2 months.
- The appearance of unpleasant sensations, for example, itching, burning, tingling.
- Violation of the integrity of the skin on the surface of the nevus. Cracks may form, from which bleeding periodically bleeds. It is necessary to pay attention to this symptom even if a diagnostic examination does not reveal the danger of degeneration of the formation. When pathogenic microorganisms enter the wound, a purulent process may occur.
- The appearance of small nodules on the surface.
- Changes in the structure of the formation, for example, compaction.
- Presence of pinpoint bleeding. It is important to pay attention to the discharge of any fluid, in particular ichor.
- Peeling.
- Hair loss (if present on the surface of the formation).
- Redness of the skin, symptoms of an inflammatory process around the nevus.
- Changing shades of nevus. You should regularly examine the skin in order to promptly notice darkening or change in color of the tumor. In case of any deviations, it is advisable to undergo an unscheduled examination for the presence of cancer cells.
Clinical signs of nevus activation
Attention! The acquisition of a different shade may indicate not only the magnesium of the nevus, but also hormonal changes in the body, the use of glucocorticoids, the formation of a cyst, injury, or the presence of an inflammatory process.
Other forms of nevus of the skin and mucous membranes
Some types of N. do not differ in morphology and structure, but have a number of wedges and features. Such N. include the Mongolian spot, nevus of Ota and linear epidermal H.
The Mongolian spot is a special type of blue N. It occurs more often in representatives of Asian peoples 1-2 days after birth in the form of bluish, bluish or brown flat spots with a diameter of up to 6-10 cm on the skin of the lumbar and sacral regions. At 4-5 years of age, the Mongolian spot gradually decreases in size and disappears.
Nevus of Ota (black-bluish oculomaxillary N.) was described in 1939 by Ota (M. T. Ota). It is a type of blue N. It is observed mainly in representatives of Asian peoples, more often in women. In 60% of cases it is congenital, in other cases it is detected in the first decade of life. It may fade somewhat with age, but does not disappear throughout life. Macroscopically, it has the appearance of a pigment spot in the zone of innervation of the I and II branches of the trigeminal nerve with dark brown pigmentation of the skin, sometimes spreading to the skin in the forehead and wing of the nose, conjunctiva, sclera and iris. In this case, pigmentation can take the form of a separate spot, or also consist of merging spots of black-gray, purple, or bluish color. Based on the severity of pigmentation and the predominant localization of the lesion, mild (orbital and zygomatic), moderate, intense and bilateral nevus of Ota are distinguished.
Linear epidermal N. has the form of a straight or oval-shaped formation in the form of pigmented nodules, separated from each other by areas of unchanged skin, figuratively compared to a string of pearls or a rosary (tsvetn. Fig. 9).
The diagnosis of various forms of N. is established by Ch. arr. based on the results of morphol, research.
Treatment
When the N. is localized in places where its accidental injury is possible, the method of choice is excision along with the surrounding skin and subcutaneous tissue, retreating 0.2-0.3 cm from the visible edge of the N. (on the face, nail bed) and 0 .5-0.6 cm (on the skin of the trunk and limbs). With giant pigmented N., in some cases they resort to stage-by-stage excision followed by skin grafting. Treatment of linear epidermal N. and hadonevus is usually caused by the need to eliminate a cosmetic defect. In this case, economical excision, diathermocoagulation (see), dermabrasion using drill cutters (see Cosmetic procedures), cryodestruction (see Cryosurgery) can be used.
The prognosis is most often favorable. However, against the background of, for example, borderline, blue N., nevus of Ota, less often with other forms, melanoma can develop (see).