Genital warts in women appear in the external genital area, causing psychological and physical discomfort. Despite the fact that these tumors are considered benign, they can lead to dangerous consequences for the life and health of a woman.
Condylomas in the intimate area
Modern gentle removal methods allow you to get rid of defects quickly and painlessly. Doctors at the Diana Clinic use the safest laser and radio wave techniques for this.
Causes of condylomas formation
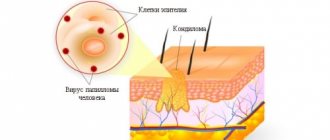
Condylomas are areas of epithelial growth on the skin of the perineum and external genitalia. They are caused by the human papillomavirus after entering the body. At first, it can behave quietly, but as immunity decreases, it provokes the growth of tumors. There are several designations for this disease : viral papillomas, genital warts. Sexual transmission is the main method of transmission of infection.
Scientists have discovered more than 100 types of HPV, 40 of which are transmitted during sex. Those most susceptible to manifestations of the disease are those with reduced immunity and chronic diseases. The growth of condylomas is provoked by strains 6 and 11. Other viruses cause warts localized on the upper and lower extremities and face. The probability of becoming infected with an infectious agent is 80%. DNA testing reveals viruses in 50% of women aged 18-25 years. However, only 10% of them encounter condylomas on the surface of the genitals. They occur in the presence of both oncogenic and non-oncogenic types of HPV.
You should be afraid of types 16, 18. And strains 31, 33, 35 are also considered unfavorable. They provoke the formation of various types of oncology affecting the cervix, vulva, and perianal area. If a sexual partner has condylomas, the risk of infection of a healthy person in contact with him is 75%. Early initiation of sexual activity is also a risk factor. Although a condom is not a 100% guarantee of protection, it still plays a positive role in prevention. It is not recommended to have sexual intercourse with a person whose health status is unknown.
The incubation period varies from 3 weeks to 8 months. On average, it lasts 3 months. HPV can remain dormant in the body for years, and sometimes throughout a person’s life. Its activation may be facilitated by decreased immunity.
Why do you need to remove condylomas?
Removal of genital warts in men and women always raises many questions among patients. The most important of them is as follows: is it worth touching the tumors at all, even if they are located in the intimate area.
Yes! Skin defects need to be dealt with for the following reasons:
- the presence of neoplasms is associated with a constant or often recurrent feeling of itching, burning, which causes significant discomfort especially when in a public place, and can also lead to sleep disturbances;
- initially benign formations in the groin area are capable of degeneration, and they degenerate into malignant tumors, which are then very difficult to fight;
- large formations are easily injured by clothing if they are located on the penis, or by feces if they are located in the anal area, which increases the risk of developing a secondary infection and can lead to blood loss;
- the presence of defects contributes to the release of a specific secretion, which has an irritating effect on the surrounding skin.
The patient should never forget that defects caused by the activity of the human papillomavirus are not only unpleasant. But they are also accompanied by serious oncogenic risks.
Popular methods for removing condylomas
Patients are wondering how the centers carry out the removal of condylomas, if organizations specialize in this.
What methods are popular and are they effective?
Today, dermatovenerologists use several different techniques to combat tumors that have developed in the intimate area due to HPV infection.
Cryodestruction
Cryodestruction is one of the most common and cheapest ways to solve the problem. To combat pathological foci, a special cooling agent is used (most often liquid nitrogen). It is applied to the problem area and, in fact, has a burning effect.
The procedure is quick and painless. When working with small lesions, it is safe in terms of leaving scars that can negatively affect aesthetics. Cryodestruction can be used to get rid of large areas of rash. If the neoplasms themselves are small in size.
To combat large formations, it is worth choosing a different method. Since the consequences of removing large condylomas in this way is the formation of scars and scars. If the procedure is performed very poorly in a large lesion, the patient may subsequently suffer from functional disorders caused by the scar or scar.
The recovery time after cryodestruction is quite long. It will take at least six months for the patient to fully rehabilitate, but the risk of relapse is quite low.
Laser therapy
Removal of anal warts, as well as formations located on the scrotum and in the immediate vicinity of the penis, is possible using a laser. However, the technique is not used directly for treating the penis.
The laser technique is also essentially burning. Instead of cold, a concentrated beam of laser radiation is used here.
Thanks to the action of which, coagulation of blood vessels in the neoplasm occurs. A skin defect deprived of nutrition dies on its own, which is the main laser effect.
The technique is used mainly for single formations or for multiple defects that are located far from each other. If problem areas cover the surface of the body with a continuous “carpet”, then the laser technique is not used at all. If after laser treatment a small scab remains on the problem area, there is no need to worry. Once the healing period has passed, the scab will fall off on its own. And underneath there will be clean skin without any negative changes.
This is interesting: HPV group a7, what is it?
Electrocoagulation
Removal of perianal, anal and some other condylomas is possible using the electrocoagulation technique. This method, like others, is based on cauterization. True, this time the thermal effect is provided not by a beam of laser radiation or extremely low temperatures, but by electric waves.
Electric waves, in contact with the skin problem area, locally increase the temperature, which leads to coagulation of blood vessels. The further mechanism for solving the problem is the same as with laser therapy.
Electrocoagulation is painful to remove condylomas
, and therefore the procedure is always performed under local anesthesia.
If the case is assessed by the attending physician as severe, then a decision may even be made on systemic anesthesia. But this is rarely required. Electrocoagulation, unlike cryodestruction or laser therapy, can be used, regardless of the number of rashes. This is its undeniable advantage. It is used in many centers involved in the removal of tumors caused by HPV. More about radiocoagulation
Removal of condylomas using the radio wave method is a relatively new word in modern dermatovenerology. The main mechanism of action of the apparatus used for manipulation is very simple.
The electric current generated by the device is concentrated on the upper part of the electrode. And then converted into thermal radiation. Thanks to this, the electrode itself essentially becomes a full-fledged radio knife. The device is called Surgitron.
Removing condylomas using Surgitron allows you to first dry out the growth and then burn it out. At the same time, according to doctors, the technique is gentle. This means that it causes minimal trauma to the skin that is not affected by the tumor. And recovery occurs in a short period of time. Removing condylomas with the Surgitron device has a number of advantages. Among which are a low risk of relapse, the ability to avoid the formation of scars, painlessness, sterility, etc.
Using the method, it is even possible to fight formations that are located inside the urethra. In addition to the mentioned approaches, there are also chemical methods for removing condylomas and surgical intervention. Both of these techniques are considered quite old and are used only according to strict indications due to their high morbidity.
Recommendations for rehabilitation after removal of condylomas
Many patients are concerned about the question of how to wash themselves after removing condylomas using the radio wave method. Or in any other way, and in general, how to provide proper care for the wound that remains after the intervention. Compliance with hygiene rules is of greatest importance in the complete and safe healing of a postoperative defect. The fact is that minimally invasive techniques usually do not leave deep wounds that require special care and long-term healing. Skin defects are small in size and can be easily regenerated.
The classic recommendations are:
- It is recommended to simply wash the genitals with water 2-3 times a day;
- if it is decided to treat the genitals with an antibacterial agent, then attention is paid not only to the site of exposure, but also to the anus, since from there the infection easily migrates to other areas;
- when washing the genitals, movements are made from front to back, which eliminates the transfer of pathogenic microorganisms from the anus;
- After treatment, the genitals should be dried with a separate towel with a soft structure.
All patients are interested in whether sex is allowed after removal of condylomas. Doctors recommend completely abstaining from sexual intercourse during rehabilitation. This, firstly, will reduce the risk of infection, and secondly, will allow the wounds to fully heal.
Diagnostic techniques
To establish an accurate diagnosis, you should consult a dermatovenerologist. He will order a test for human papillomavirus using the polymerase chain reaction method.
This is a fast and very informative method, which uses diagnostics at the molecular level. To detect the papilloma virus, a genital smear is usually taken. The manipulation takes a few minutes and is not accompanied by pain. This analysis is carried out to determine the amount of virus and identify its specific strain.
Laser removal of blood vessels
| Name of procedure | Cost, rub | |
| Primary consultation with a dermatovenerologist, cosmetologist | 1 000 | |
| Repeated consultation with a dermatovenerologist, cosmetologist | 500 | |
| Laser removal of hemangioma, blood vessels, pigmentation | up to 1 cm / from 2 | 500 / 400 |
| Laser removal of blood vessels, pigmentation, rosacea, rosacea | nose | 2 000 |
| Laser removal of blood vessels, pigmentation, rosacea, rosacea | cheeks | 4 000 |
| Laser removal of blood vessels, pigmentation, rosacea, rosacea | chin | 2 000 |
| Laser removal of blood vessels, pigmentation, rosacea, rosacea | face | 6 000 |
| Laser removal of blood vessels, pigmentation, rosacea, rosacea | neck | 4 000 |
| Laser removal of blood vessels, pigmentation, rosacea, rosacea | neckline | 4 000 |
| Laser removal of blood vessels | shins / thighs | 8 000 |
| Laser removal of blood vessels | feet | 6 000 |
| Laser removal of blood vessels | legs (no feet) | 16 000 |
================================================================================
Removal of warts, condyloma, papilloma, moles
Important! If you find yourself with genital warts, you should get tested for STIs.
Need for removal
It is mistakenly believed that removal of condylomas in the intimate area allows you to forget about such a delicate problem forever. But it is impossible to remove the pathogenic microorganism. It remains with the person forever and is activated when appropriate conditions arise. It is possible to cope only with the external symptoms of the pathology. In this regard, patients often wonder whether it makes sense to remove genital warts if this is not a treatment. But this is necessary, and not only for aesthetic reasons. Why deletion is justified:
Condylomas provoke burning and itching near the anus and in the intimate organs, causing a person to experience discomfort. There is a risk of traumatizing the growths with items of clothing, which can lead to bleeding and pain. If this happens, there is a possibility that the tumor will degenerate into a tumor. Large growths become a source of unpleasant odor due to the release of fluid that irritates the skin and mucous membranes. This secretion of condylomas provokes inflammation of the epidermis.
Condyloma is initially benign in nature, but gradually can lead to oncology. This is explained by the tendency of the papilloma virus to mutate.
It turns out that condylomas must be removed, but this should be done competently and safely for health. For this purpose, it is necessary to contact an experienced dermatologist. There are several methods available, and they depend on the size of the formations and their location.
View full version: Condylomas grow rapidly after laser
Hello, dear doctors! I already asked a question about condylomas. 35 years. HPV 51. There are no other sexually transmitted infections. There are no other chronic diseases. Condylomas were removed with a laser. Two weeks after removal, everything looked clean. After menstruation, the burning sensation during sexual intercourse reappeared. And they sprinkled condylomas - everything is dotted with them in the place where the labia minora closes from below, in the fold, before our eyes they increase in size and rise higher in area. Before removal there were two scallops, now they simply cover the affected area in a solid mass.
1. Could the laser lead to infection of surrounding tissues (the situation was stable before the laser)? 2. Should laser cauterization somehow protect healthy areas of the mucous membrane? 3. It is necessary to remove it now, as I understand it, otherwise everything will be overgrown with them and then how to carry out the operation? Is there a safer removal method?
By the way, contrary to what I read here on the forum, the burning sensation is definitely caused by condylomas. It is enough to run your finger over the area of infection to understand this - the burning sensation seems to be caused by mechanical irritation of the bases of these condylomas.
Please advise what to do now and who to contact in St. Petersburg. And how to conduct a sexual life if, apparently, you will have to remove them once a month: that is, there is either constant discomfort and the presence of the formations themselves does not add an intimate atmosphere, or in the interim, a state after removal, when sexual life is excluded. Can this really last for the rest of my life, given my age?
So liquid nitrogen? I abandoned this method as ineffective (I spent a long time reading reviews). Thanks, I'll try anyway.
Hello! The condylomas have started to bleed a little, but my doctor still insists that they are very small and there is no need to rush into re-intervention. That you can burn the mucous membrane like that. I took a smear for flora - it was normal. To heal cracks in condylomas, the doctor prescribed Levomekol. I started using it and looking in the mirror I discovered that there were still cracks on the labia minora near the clitoris and between the labia minora and labia majora. After using levomekol it became even worse. It hurts to touch your lips and it’s unpleasant to sit.
Now I apply d-panthenol, it doesn’t help. What could these symptoms be?
Is it really impossible to frequently influence the mucous membrane in order to remove condylomas? I want to get rid of them completely.
Should I see a dermatologist instead of a gynecologist?
This is interesting: Vitamins for HPV 16
Cracks can serve as “gateways” for the penetration of the virus, and you should try to avoid any injuries (therefore, this must be taken into account, since cracks often appear during “traumatic” sexual intercourse). Unfortunately, if there are a lot of small genital warts on the vulva, then it is not possible to completely remove them, and removing visible rashes does not ensure complete removal of the virus from the skin and mucous membranes (monkey labor associated with pain and material expenses for you). Calm down and live with genital warts for a while. Usually, in the vast majority of cases, it is one or two years, sometimes up to several years. Over time, as it multiplies, the amount of the virus will increase so much that it will become possible for it to be recognized by your body’s immune system, after which the immune system itself, and almost painlessly, will destroy genital warts and cleanse your body of this virus.
Dermatovenerologist, Fediy Bogdan Nikolaevich.
Cracks can serve as “gateways” for the penetration of the virus, and you should try to avoid any injuries (therefore, this must be taken into account, since cracks often appear during “traumatic” sexual intercourse). Unfortunately, if there are a lot of small genital warts on the vulva, then it is not possible to completely remove them, and removing visible rashes does not ensure complete removal of the virus from the skin and mucous membranes (monkey labor associated with pain and material expenses for you). Calm down and live with genital warts for a while. Usually, in the vast majority of cases, it is one or two years, sometimes up to several years. Over time, as it multiplies, the amount of the virus will increase so much that it will become possible for it to be recognized by your body’s immune system, after which the immune system itself, and almost painlessly, will destroy genital warts and cleanse your body of this virus.
Dermatovenerologist, Fediy Bogdan Nikolaevich.
Bogdan Nikolaevich, thank you for your answer. But there was no “traumatic” sexual intercourse. Even the burning sensation inside the vagina, which bothered me when genital warts appeared, has gone away.
It really cracked everywhere, about 8 cracks from 1 to 3 cm long. Only one is quite deep, the rest are superficial.
I definitely won’t see a doctor before the holidays are over. I decided to smear them with zinc paste for now (it was the only one that once helped me with cracks and peeling around my mouth). Isn't this self-medication harmful?
And one more thing: can another infection manifest itself this way, for example. herpes-2? It was not detected by PCR, and nothing except HPV. Is it worth looking?
Of course, I want to believe that condylomas will disappear, but, for example, ordinary papillomas on the body (I have several of them) do not go away on their own for about 10 years. And laser removal is almost painless (anesthesia is a spray), and I have a low pain threshold. I don’t know the truth about the effectiveness, I think everything about liquid nitrogen, but the current state of the mucous membrane worries me greatly, whether it will get worse.
Bogdan Nikolaevich, thank you for your answer. But there was no “traumatic” sexual intercourse. Even the burning sensation inside the vagina, which bothered me when genital warts appeared, has gone away. It really cracked everywhere, about 8 cracks from 1 to 3 cm long. Only one is quite deep, the rest are superficial. There must be some reason for the cracks to appear? We need to deal with this. Eliminate provoking factors. For healing, you can use ointments or creams with antibiotics. Of course, I want to believe that condylomas will disappear, but, for example, ordinary papillomas on the body (I have several of them) do not go away on their own for about 10 years. . Papillomas on the body, the so-called acrochordons, have nothing to do with viral warts (genital warts), are not associated with HPV, and are peculiar growths on the skin that do not resolve on their own.
Dermatovenerologist, Fediy Bogdan Nikolaevich.
There must be some reason for the cracks to appear? We need to deal with this. Eliminate provoking factors. For healing, you can use ointments or creams with antibiotics.
Dermatovenerologist, Fediy Bogdan Nikolaevich.
The levomekol made it worse; I applied it for about 2 weeks.
What other directions should we look in? HPV itself cannot cause such symptoms? It began with an active burning sensation, and only then condylomas appeared, but there was a feeling that some kind of inflammation was present and microcracks accompany even the smallest of condylomas. But they also appear in places where there are no condylomas visible to the eye.
How to exclude provoking factors - this is only if you exclude sex life, walking, etc. altogether. ?
Can candidiasis manifest itself this way if there is no plaque?
I am writing for those who encounter a similar problem. It was still a FUNGAL INFECTION. Absolutely all tests did not show it! It got to the point where sexual life became completely impossible due to itching, burning, swelling, and the labia hurt (namely, they hurt, like a sore throat or a bruise) on their own. I went to the doctor again, they didn’t say anything definite, I had smears, etc. As a result, my patience ran out and I took 150 mg of fluconazole + applied clotrimazole externally. In the morning, the symptoms of swelling stopped, and by the evening of the second day, touching the condylomas was NOT PAINFUL. This means that the cause of pain and burning is not condylomas. I think that the condylomas themselves appeared due to chronic candidiasis. I am going to undergo the maximum course of treatment, and then remove the condylomas again.
This is interesting: HPV testing for cervical erosion
Question for doctors: after removal of condylomas, antibacterial suppositories are prescribed prophylactically, which can again cause thrush. Is it possible to replace them with something? Are they necessary?
Condylomas spread very quickly. Three months after the first removal, cauliflower grew on both sides of the vaginal opening. After the second removal, there was a larger area of burns, and healing was much slower. And they keep growing! I looked in a magnified mirror - I don’t see any free mucous membrane on the labia at all, either there is already a noticeable roughness, or there are barely noticeable bulges in paths. Before the disease, all these places were absolutely smooth.
Small ones cause a burning sensation and are painful to the touch. Sexual life stopped completely due to painful sensations and especially due to the psychological state.
To what extent can this continue? If all the mucous membrane is burned out with a laser, will they stop growing? What will happen to the mucous membrane? Will this continue for years? Does this condition mean that the virus will definitely not go away?
All smears are normal. I took it 4 times over the past six months in different phases of the cycle.
I am 36 years old, a little over a year since the first condyloma appeared. HPV 51.
Methods for removing growths
Destructive methods for treating papillomavirus are divided into physical and chemical. In any case, the goal is the same - removal of growths. In the first case, the neoplasm is removed with the chemical compositions Solcoderm and Solkovagin. As for physical methods, the following are available today:
- Electrocoagulation. It involves getting rid of warts using electric current. Pain is considered the only drawback of this technique. After the procedure is completed, the wound may take a long time to heal, causing discomfort. Cryodestruction. Here liquid nitrogen is used to freeze the condyloma. This method involves treating external tumors, but is not suitable for growths that are localized internally, for example, on the cervix. At the end of the procedure, ulcers are formed that heal without scarring for 2 weeks. It takes 6 months to achieve complete restoration of the skin.
- Laser therapy is the best method for removing growths. The surgeon uses a special laser to remove genital warts. The use of this method is minimally traumatic and does not leave scars. The rays can penetrate to any depth. This method is suitable for both individual growths and those that have merged together. Laser removal of condylomas is possible if they are located on the cervix. After such an intervention, the rehabilitation period is no more than 1 month.
- Radiosurgery is a popular method in which a special radio knife excises damaged areas. During manipulation, it is possible to take material from the wart to examine it. The radiosurgery method is considered the best in terms of preventing relapses. The most traumatic is considered to be surgical, when the doctor uses a scalpel. Despite the popularity of this method, it is considered the most effective. After such an operation, the recovery period takes about 2 months.
A recovery period is provided for any surgical option. Its duration varies and depends on many factors. The patient will have to stop lifting heavy objects for a while. Sexual activity and exposure to direct sunlight are prohibited.
Application of liquid nitrogen
This method is called cryodestruction and consists of crystallization of the intercellular fluid present in the structure of condylomas. Treatment with liquid nitrogen damages them and they gradually fall off.
To carry out this manipulation, the doctor uses an applicator. He dips it in the active ingredient (liquid nitrogen). After this, he applies the drug to the condyloma and leaves it for 30 seconds. The procedure is not painful, but sometimes there is a small scar. The durability of the result and its effectiveness can be described as average.
Thermal methods and use of radioknife
Thermal methods of destroying condyloma are painful. Before they are performed, an anesthetic is required to be injected into the area with the growth. A person may complain of pain for several days after the procedure. We cannot exclude the possibility that a scar will remain after removing the growth. Despite all these disadvantages, the method is very effective and promotes lasting results.
Destruction using a radio knife involves the use of the Surgitron apparatus. It generates electromagnetic waves. Sometimes, with the help of such equipment, it is possible to combine the use of electrocoagulation and a radioknife. The latter contributes to the destruction of the pathological area, while electrocoagulation seals small vessels. This is a fairly effective method, but the durability of the results is average.
Laser ray
To implement this method, a carbon dioxide laser is used. The consequence of this procedure is a microscopic wound that heals within a month. The accuracy of genital wart removal is the main advantage of this method. Adjacent areas of skin are not damaged.
Thanks to the independent restoration of the epidermis, there is no rehabilitation period. Laser treatment is carried out on formations on open and closed areas of the body, including delicate areas. Laser removal of condylomas is contraindicated if there is local inflammation on the skin, open lesions, as well as infectious diseases, herpes.
The procedure is performed under anesthesia and is therefore considered painless. But after the drug wears off, the patient may experience slight pain. During laser radiation, light penetrates the tissue and is instantly absorbed. Next, light energy is converted into heat. However, the fluid in the condyloma cells evaporates. The neoplasm is destroyed. The main advantages of laser destruction are:
- Safety. Using a laser eliminates the possibility of infection getting into the wound. Any complications are kept to a minimum. During the recovery period, the patient does not have to deal with wound suppuration and inflammation.
- Minimal trauma. The laser beam acts directly on the condyloma. Healthy areas are not affected either in depth or in breadth. Due to this, the treated area heals quickly.
- Gentle action. Laser therapy is a gentle and at the same time radical technique for removing condylomas. It can also be used on sensitive areas, for example, in the perineal area.
- No blood. Laser radiation promotes disease of small vessels, so the method is considered bloodless.
Laser therapy is suitable for both young patients and adults. It is allowed to be carried out by both women and men.
Removal of condylomas on the penis
Removal of condylomas with liquid nitrogen on the penis is carried out after consulting a doctor.
If necessary, the doctor prescribes a biopsy of the tumor to exclude an ongoing malignant process.
The cryodestruction procedure can be carried out in several ways - using a special device and manually.
The first method involves exposure to cold using a cryoprobe.
The second method is more often practiced in cosmetology clinics with the aim of removing single skin lesions.
When manually removing condylomas with nitrogen, damage to adjacent tissues and re-growth of tumors are most often observed.
Hardware cryodestruction allows you to most accurately influence pathologically altered tissue without damaging the healthy epidermis.
In addition, the specialist has the ability to control the depth of nitrogen exposure, which ensures high efficiency of the procedure.
Genital condylomas in men most often affect the foreskin and head of the penis, and can be found on the body of the penis.
If left untreated, the tumors spread, affecting the scrotum and anal area.
Benefits of removing genital warts on the penis with liquid nitrogen:
- There is no need for special training.
- The duration of the manipulation does not exceed 15-30 minutes.
- Compared to other modern methods, cryodestruction has a relatively low cost.
- The risks of bleeding or infection are practically zero.
Among the disadvantages of cryodestruction of condylomas on the penis, the following points can be highlighted:
- Discomfort, slight pain (if necessary, done using local anesthesia).
- There is a possibility of burns and marks appearing after complete healing of the epithelial tissue.
- Sometimes there is a need for repeated cryomanipulation.
The procedure is not recommended for men in the following cases:
- Intolerance to liquid nitrogen (presence of an allergic reaction to the substance).
- Acute neurological diseases accompanied by epileptic seizures.
- Diseases of the cardiovascular system in the acute stage. Infectious and inflammatory pathologies of the urogenital tract.
- Wounds, damage to the skin on the body of the penis.
- Atypical (malignant) formations.
When removing genital warts with nitrogen, the following side effects may be observed, which are not considered complications:
- Formation of a bubble at the site of application of liquid nitrogen. The reaction is absolutely normal; over time, the bubble turns into a crust and disappears on its own.
- Swelling of the skin around the removed condyloma. The reaction does not require special treatment; tissue swelling goes away on its own after 2-5 days.
The manipulation to remove HPV formations is carried out in the office of a dermatovenereologist or urologist.
The man is asked to lie down or sit on the couch.
Next, using a cryoprobe or a sterile cotton pad, nitrogen is applied to the condyloma.
When manually removing warts or papillomas from the surface of the penis, the doctor dips a cotton swab in liquid nitrogen and then applies it to the formation for 5-30 seconds.
After a few minutes, the condyloma thaws, and the doctor has the opportunity to evaluate the effectiveness of the procedure.
After the manipulation, the patient may notice the appearance of a bubble.
A week later it bursts and a crust appears in its place, which will subsequently fall off.
After the crust peels off, a new, healthy epithelium appears.
Potential Complications
It is not recommended to remove condylomas yourself at home. This is unsafe and does not always lead to the expected effect. To successfully cope with such a procedure, it is necessary to understand the mechanism of manipulation and have theoretical knowledge. Instead of dubious folk remedies, it is better to give preference to treatment with the presence of medical personnel. This will reduce the likelihood of complications to a minimum. Adverse consequences of the procedure may include the spread of infection to healthy areas of the skin, the formation of unsightly scars, and pain in the treated area.
If, after removal of condylomas, a woman decides to become pregnant, she should first consult a gynecologist. He will determine the patient’s immune status and select an individual medication plan for her, if required. Typically, specialists prescribe antiviral agents and immunomodulators for prevention. If itching and discharge appear as a result of removing growths, this may indicate an inflammatory process. Subsequently, new warts form due to this. To avoid encountering genital warts, you should follow your doctor’s instructions and adhere to preventive measures.
How to prepare for removal of genital warts?
No special preparation is required for removal, but following simple recommendations makes this procedure easier for the woman.
Before removal, doctors recommend:
- visit a gynecologist;
- donate blood for analysis to detect specific immunoglobulins and signs of inflammation;
- undergo PCR diagnostics to accurately determine the type of pathogen;
- do not use intimate cosmetics and intimate hygiene products on the eve of the procedure (carry out hygiene with clean water);
- do not visit the sauna, bathhouse, solarium for 2-3 days;
- stop taking medications that interfere with blood clotting.
To avoid complications, it is important to tell your doctor if you are allergic to anesthetics.
Skin care
After removing the condyloma, it is necessary to avoid skin contact with water. It is prohibited to smear creams on it or use decorative cosmetics. During the recovery period, a crust appears on the surface of the growth. It must not be torn off, otherwise infection will penetrate into the open frame. Even if infection can be avoided, the healing time will be delayed. In addition, the formation of a rough scar cannot be ruled out. The crust should come off on its own.
When this happens, you should protect the epidermis from direct sunlight by applying a cream with an ultraviolet filter. This approach will avoid the formation of age spots. The use of a washcloth is prohibited until the crust completely falls off.
How can you remove condylomas?
The development of technology provides more and more opportunities for this. Moreover, the most traumatic method, which consists in getting rid of growths surgically, is used less and less. It is being replaced by virtually painless hardware methods that minimize tissue injury:
- Cryodestruction. The peculiarity of the method is the effect on the growth at very low temperatures. They are usually caused by skin contact with liquid nitrogen, although other coolants may be used. Compared to other methods, cryodestruction can be called the longest method of exposure to infected tissue, but it always gives a 100% result. Its essence is as follows: liquid nitrogen is injected under the skin at the location of the condyloma, which gradually causes the growth to be rejected. During the procedure, almost no pain is felt: only a slight burning and tingling sensation is possible. Pain may appear a little later - in the first hours after cryodestruction. Then swelling and redness appear at the treatment site, a bubble appears, which bursts on its own within a week. Then all that remains is to wait until the HPV-infected tissues die off - this will happen in a maximum of a month and a half - and the wound will heal completely. At this time, it is recommended to use an antiseptic - it will be prescribed by a doctor.
- Coagulation with radioknife. High-frequency radio radiation directed at the location of the condyloma leads to evaporation of the tissue. With this approach, condyloma removal is carried out very quickly under local anesthesia. In this case, the tissues located nearby are not injured. The method is also very good in that rehabilitation as such after the procedure is not needed. But radio wave coagulation has a number of contraindications, which include pregnancy and lactation, the presence of an acute inflammatory infection, diabetes mellitus, a pacemaker, and oncology.
- Laser coagulation. A relatively young method, the method of action is similar to coagulation with a radioknife. Condyloma removal occurs in a non-contact manner thanks to the use of laser beams of different lengths. The patient does not feel any pain or discomfort at all. Rehabilitation takes about a week - during this time you cannot visit bathhouses, swimming pools, or open reservoirs. During this time, a crust appears on the wound, which then disappears. You should also, if possible, avoid exposure to direct sunlight. To the contraindications mentioned above, one should add disturbances in the functioning of the immune and endocrine systems, and a tendency to thrombosis.
- Coagulation with a heated electrode (common name - cauterization). Often used for small condylomas. When the electrode touches the tissue, a burn appears, which within an hour becomes covered with a dark crust. Then, within a week, the crust disappears. The method is proven and reliable; its advantage is that blood vessels are “sealed” simultaneously with the tissues, which completely eliminates the risk of bleeding. In addition, the skin and wound are disinfected naturally, which is understandable due to the exposure to high temperature.
Laser irradiation of condyloma
Prevention measures
In most cases, the virus is transmitted sexually. This is why it is important to avoid casual relationships. During sex, it is necessary to use barrier methods of contraception. It is necessary to maintain personal hygiene, because infection sometimes occurs in domestic conditions.
Strong immunity and a healthy lifestyle will make it possible to avoid the formation of condylomas and papillomas in the future. It is important to be examined promptly and undergo laboratory tests if the need arises. HPV may not manifest itself for a long time while in the human body.
How much it costs to remove condylomas depends on the size of the tumor, the number of growths and the pricing policy of the clinic. Removal of large tumors (0.5 cm), together with an appointment with a dermatologist and pain relief, will cost 2500-3500 rubles.
What does genital papilloma look like?
The disease manifests itself after a week as tubercles. Fabulas affect the intimate areas of women. Such neoplasms are grouped around the penis of men.
A photo of genital papillomas shows an image resembling the sharp comb of a rooster. Strains 6, 11, 13, 16, 18 are the cause of ill health. They can fester and become ulcers.
Thread-like - appears as a yellowish protrusion on the eyelids, neck, armpits. Then it takes on the appearance of a thread and lengthens. It becomes a six-millimeter elongated neoplasm. Sometimes they become inflamed.
Other types of sex
Due to the fact that transmission of the virus can occur through the use of condoms, the best way to protect yourself is to avoid sexual intercourse.
When a patient does not stop having sex with condylomas, it is worth adhering to the following rules:
- Using condoms. The method, although not 100% protective, can significantly reduce the threat of the spread of the virus. The possibility of infection remains due to the inability of a condom to protect the surface of the skin or mucous membranes of the genitals from contact.
- Before engaging in sexual contact, you should not be embarrassed to discuss the disease with your partner. He may not be aware of the presence of the virus and the threat of its spread.
- If symptoms of HPV are detected, contacts should be reduced and sexual activity should be stopped for the period of treatment.
- Do not have sex with an infected person.
- Don't change partners. The threat of infection increases in proportion to their number.
Papillomavirus is transmitted by people who have oral and anal sex. For the virus, it is not the organ that is important, but contact with the mucous membrane. A blowjob with an infected person is a great opportunity to become infected. Using a condom during oral sex reduces the risk of infection, but does not eliminate it completely.
The following types of condylomas are known.
Pointed
These formations are small growths on the stalk. Condylomas are small and rarely isolated. They usually grow in colonies with a tendency to merge into one formation. They often appear in intimate places, they are also called genital. When considering this type of condylomas, it is necessary to highlight the main points:
- In almost 90% of cases, infection occurs during sexual contact;
- the virus is transmitted to the child during birth;
- condylomas do not appear for years.
IMPORTANT: You should know that genital warts are considered a symptom of papillomatosis. But strong immunity will keep the virus dormant for a long time.
Flat
This name is explained by the fact that such condylomas are characterized by a slight elevation above the skin. Their symptoms do not appear for a long time, and they do not look scary.
The growths do not hurt, the size does not exceed 5 mm, and the color is like healthy skin. The only thing that irritates is their multiple scatterings.
If flat condylomas appear, you should immediately seek medical help. Such formations often serve as an impetus for the formation of malignant tumors.
Over time, typical symptoms appear:
- unbearable itching;
- burning;
- the area of neoplasms begins to turn red;
- the affected areas become inflamed.
If the manifestations are not treated, the condylomas will begin to grow, covering large areas.
Wide
Such formations indicate the presence of pathological conditions that cause serious consequences. The main reason for their appearance is considered to be syphilis, enhanced by the papilloma virus.
In the first stage of formation, wet blisters are observed on moist areas of the body. Then they begin to burst, forming ulcers. Wide condylomas form on the wounds. Gradually they increase in size and expand their localization.
Dermatologists say that this type of condylomas is the most insidious skin manifestation. In addition to sexual transmission of the disease, infection also occurs through household means.
ATTENTION: Condyloma lata contains Treponema pallidum, which is the causative agent of syphilis. Therefore, the carrier of the virus is able to infect others without even knowing it.
Treatment of papillomas, condylomas (HPV)
- performed on the body by a dermatologist-cosmetologist,
- on the male genitals - urologist,
- for women - a gynecologist,
- in the area of the anus and perineum - proctologist.
There is now a treatment that is highly likely to eliminate HPV infection. Modern treatment for genital warts can not only remove or reduce the symptoms of the disease, it eliminates the HPV infection and prevents further transmission of the virus in many cases. However, after any treatment method, relapses are possible.
- Laser removal of genital warts is performed under local anesthesia.
- Electrocoagulation, removal of genital warts using high temperature, is carried out under local anesthesia.
- Interferon blockades (genital warts are injected with an interferon drug).
- Radio wave removal of condylomas. Today, the most effective method for removing genital warts. There is no trace left of condylomas.
Forms and symptoms of the disease
There are several types of genital warts: flat, keratinized, papules and genital warts. The growths appear not one at a time, but in groups. This phenomenon is called condylomatosis.
Condylomas, which grow on mucous layers, are distinguished by a pointed, but at the same time soft surface. They are formed on a base called a stalk.
The outer surface of the tumor depends on its location. On the outside of the genitals they take the form of a papule, which is quite dense. There are keratinized areas on it. They look like thread-like growths on the very surface of the wart. In the fold of the buttocks and in the groin, condylomas are located above the surface of healthy skin. Their layer is uneven. In this area they are constantly subjected to rubbing, so that they become damaged and bleed.
As a result, this disease is accompanied by a secondary type of infection. If growths appear on the vulva, they are distinguished by a whitish tint or, conversely, become brown.
If they are located on the mucous layer, then their color is reddish or pinkish.
As a rule, condylomas of this type are formed in those areas where tissues are most often injured during sexual intercourse. The incubation period can last from a couple of weeks and extends to several years. During this time, the infection develops. The incubation stage is the period from infection to the appearance of the first signs of the disease.
After this, pinkish or flesh-colored growths appear on the human genitals. Their sizes vary from 1 mm to 40 mm. They are gradually growing. They usually appear in groups of several growths. Often such neoplasms merge into a single growth, which resembles cauliflower in appearance.
In women, genital warts are most often located on the labia minora and labia majora. They can also spread to various transverse folds of the skin. They then move to the clitoris, vagina, cervix and urethra.
In men, genital warts usually form on the head of the penis. They can also grow on the foreskin and frenulum. Often such neoplasms look like necklaces of papules, 1-3 rows near the head of the penis.
In both men and women, growths appear near the anus. However, such a location does not always depend on anal sex. Typically, the virus does not affect a limited area of the human body, but the entire perineum, inguinal folds and the area near the anus.
Patients often experience itching and irritation. The pain is not intense. Sometimes there is difficulty during sexual intercourse or walking. The most severe form of the disease occurs in people who suffer from diabetes, pregnant women, HIV-infected people and people taking immunosuppressants.
Where to undergo destruction of genital warts (papillomas) in Moscow?
In a multidisciplinary medical center you can always perform the destruction of genital warts (papillomas)
. Our medical center is located between the Konkovo and Belyaevo metro stations (South-Western Administrative District of Moscow in the area of the Belyaevo, Konkovo, Teply Stan, Chertanovo, Yasenevo, Sevastopolskaya, New Cheryomushki metro stations " and "Trade Union"). Here you will find highly qualified personnel and the most modern diagnostic equipment. Our clients will be pleasantly surprised by our quite affordable prices.
Timonina Ekaterina Sergeevna
Obstetrician-gynecologist, gynecologist-endocrinologist, ultrasound specialist (ultrasound) More than 10 years of experience