Rubromycosis on the leg
The fungal disease rubromycosis is a common disease that mostly affects the skin of the feet, palms, and provokes the destruction of nails. In rare cases, it is diagnosed on the skin of the head, face, or deep folds in the groin or under the breasts in women. In advanced conditions, rubromycosis on the leg causes inflammation of the vellus or long hair follicles in humans.
What causes the disease
The main fungus that causes rubrophytosis is an anthropophilic pathogen. It is an intermediate formation between epidermophytons and trichophytons. This means that its spores equally affect human skin or hair.
This species of fungus is very common in normal environments and has a high degree of activity under favorable conditions. Depending on the state of the immune system and the endocrine system, the following may form:
- rubromycosis on the leg (feet);
- rubromycosis of nails;
- rubrophytosis of the hands;
- generalized form of rubromycosis.
One of the features of this type of fungus is its ability to penetrate the skin and be transmitted throughout the body by the lymphatic route. It does not have a clearly defined incubation period. Good immunity and good health can restrain its development indefinitely.
Treatment of the disease
After identifying the pathogen, they proceed to the treatment of rubromycosis of the nails. The infection can be eliminated with drug therapy. Both local and systemic antifungal drugs are used.
Local preparations
The arsenal of drugs for external use is wide. For rubromycosis of the feet and nails use:
- 1% cream, ointment, solution Clotrimazole (clotrimazole) Glaxo-Wellcome Poznan (Poland);
- Cream, lotion Mifungar (oxinazole) Zentiva (Czech Republic);
- 1% ointment, solution Exoderil (naftifine) Sandoz GmbH (Austria);
- 1% ointment, solution, cream Mycospor (bifonazole, urea) Kern Pharma (Spain);
- 10% solution, ichthyol ointment (ichthammol) Tula Pharmaceutical Factory (Russia);
- 1% solution of brilliant green dye (tetraethyl-4,4-diaminotriphenylmethane oxalate) SnezhPharm (Russia);
- Fukortsin solution (boric acid) Tula Pharmaceutical Factory (Russia).
- 0.1% Locoid ointment (hydrocortisone) Brocades/Yamanouchi (Netherlands);
- 0.1% ointment Gentamicin-AKOS (gentamicin) Synthesis AKOMP (Russia);
- 2% cream Pimafucin (natamycin) Brocades/Yamanouchi (Netherlands);
- 1% cream, varnish Batrafen (ciclopirox) Sanofi-Aventis Deutschland GmbH (Germany);
- Lac Loceryl (amorolfine hydrochloride) Galderma Laboratories (France).
The duration of treatment with local drugs can be from 1 to 4 months. Treatment is continued until the external symptoms of the fungus are completely eliminated.
Read more Itching in the anus which doctor
System Tools
External treatment of nails and feet with drugs may be ineffective due to the active proliferation of infection. In such situations, mycologists prescribe oral drugs with antifungal and antihistamine effects:
- Tablets Nizoral (ketoconazole) Janssen-Cilag (Italy);
- Orungal capsules (itraconazole) Janssen-Cilag (Italy);
- Tablets Diflazon (fluconazole) JSC KRKA, d.d., Novo Mesto (Slovenia);
- Tablets Lamisil (terbinafine) Novartis Consumer Health SA (Switzerland);
- Fulcin tablets (griseofulvin) Pharm Group (UK);
- Capsules Sporanox (itraconazole) Janssen (Italy).
Nail removers
In order to accelerate the peeling of deformed nails and remove the main accumulations of fungal spores, keratolytic agents are used:
- Trichloroacetic acid;
- Salicylic acid;
- Urea.
They have a softening effect, thereby making it easier to remove affected nails using nippers. The procedure is performed once a day. Treated nails are sealed with adhesive tape.
Keratolytic properties are characterized by:
- Ointment containing potassium iodide;
- Ointments with lanolin.
After applying a thick layer of ointment, cotton wool is applied to the nails and the fingers are bandaged. The bandages are worn for 3 days. If necessary, repeat the procedure.
Main clinical symptoms
Rubrophytia photo
This disease is most often diagnosed among fungal skin lesions. Dermatologists note that in 70% of cases when people turn to them for help, tests show the presence of anthropophilic fungi or spores. In most cases, rubromycosis on the leg begins on the smooth surface of the foot or palm, immediately moves to the interdigital folds, and brings great discomfort when walking.
Among the most common and characteristic symptoms, patients note:
- increased dryness of the arch of the foot or hands;
- redness of the skin is observed;
- the pattern on the surface of the palms becomes clear and prominent;
- increased peeling begins, which in structure resembles flour.
In the absence of proper treatment, damage to the lateral surface begins, peeling and redness spreads over the entire foot or hand. Nails are involved in the process.
Rubrophytosis of the nail plates always occurs against the background of a fungal disease of the skin areas nearby. The main symptoms of this problem are:
- nails begin to exfoliate intensively;
- the shape changes, curvature or ingrowth into the soft tissue occurs;
- the plate thickens and begins to crumble.
- All fingers are always involved in the process.
Rubromycosis on the heel
When the disease first affects the free edge and sides of the nail, the entire upper part is covered with thin grooves. They are destroyed to an extreme degree and only small parts of the stratum corneum remain near the skin fold. Patients begin to have problems with gait and choosing comfortable shoes.
External signs
The photos below of rubromycosis of the feet and nails show what the fungal disease looks like in various forms of manifestation.
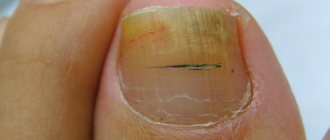
Nail damage
In the normotrophic form of the fungal infection, the oval of the nails remains the same, the pale pink color of the plates is diluted by white or yellowish longitudinal stripes.
With hypertrophic rubromycosis, the affected nail plates are dry, thickened, brittle, and crumble easily. Their color is different from the original, characterized by pronounced yellowness with admixtures of gray shades.
The atrophic form of nail rubromycosis is characterized by complete destruction of deformed nails. The plate takes on an ugly shape and completely lags behind the base. The remaining small part of the nail at the nail fold indicates that even the loss of the nail plate cannot stop its further restoration - growth.
Foot lesions
https://www.youtube.com/watch?v=_R0UbjUvrTc
Scaly rubromycosis is recognized by peeling of the sole and its redness. The foot becomes rough and small cracks appear on its surface.
The squamous-hyperkeratotic form of fungal foot disease is characterized by an increase in the number of pityriasis scales, the epidermis is markedly inflamed, and the pattern of the sole is excessively distinct due to a whitish coating.
Interdigital rubrophytosis manifests itself in a violation of the integrity of the interdigital epidermis. It is thickened and a rash appears on it. The skin bursts and peels off.
The dyshidrotic form is characterized by the appearance of a blistering rash on the sole. The lesion has a purplish pink color. Dark brown spots form in places where the bubbles have opened.
Damage to nails and feet by rubromycosis
Generalized form of the disease
Advanced or generalized rubromycosis
In the absence of comprehensive treatment of local forms of rubromycosis, its generalized stage may develop on the leg. Its main cause is decreased immunity and exacerbation of chronic diseases. It accounts for at least 25% of all visits and most often spreads through the lymph nodes and bloodstream. At this stage, large folds are involved in the process: inguinal, intergluteal or under the mammary gland. This is more typical for people who are overweight and sweat excessively.
Distinctive external signs of the generalized form:
- the lesions are visible as if from within the layers of the skin;
- the affected areas turn brown, and active powdery peeling begins;
- a small cushion forms around the inflamed area;
- the edges of the roller become covered with crusts and rashes.
This form is characterized by unbearable itching, which is difficult to relieve with conventional antimycotic drugs. It often becomes chronic and greatly bothers the patient in the warm season, after suffering infections and colds.
Types and symptoms
Rubrimycosis of the feet
With it, the skin of the feet has a slightly reddened tint, thickening, dryness and flaking appear. Manifestations are accompanied by a number of rashes and itching.
If urgent treatment measures are not taken, rubromycosis of the feet will spread to the nail area and other parts of the body.
Rubrimycosis of nails
When one nail plate is affected, all are affected. Rubrimycosis of the nails can be detected by the following signs:
- Thickening of the nail. This sign refers to the hypotrophic type of damage to the nail plate.
- Nails change from a healthy shade to yellow-gray or gray-white. This characteristic occurs in the normotrophic stage.
- The nail plate becomes fragile. This indicator is associated with the atrophic type.
There are several types of smooth skin diseases:
- erythematous-squamous;
- follicular nodular;
- infiltrative-suppurative.
A distinctive feature of the first type is considered to be a change in the healthy color of the skin to red-pink spots. In advanced cases, the color of the lesion becomes brown, increases in size, and peeling is observed.
With the follicular-nodular type, the area of vellus hair begins to be affected, as a result of which the shine disappears, the hair appears dull and brittle.
Even after the end of the disease, scars may remain in the affected area, which refers to the last type of pathology of smooth skin.
When the incubation period of the fungus ends, damage to the interdigital folds (all) is noted. Once these areas become infected, the dermis on the sole becomes infected. The development of infection is indicated by the following external symptoms:
- the pattern on the dermis becomes clearer;
- the dermis becomes dry;
- mucoid peeling is visible;
- diffuse hyperemia.
Without proper therapy, the infection spreads to the back, side of the foot, and toes. The universality of the development of pathology in children is the presence of exudation, which complicates the diagnosis of the disease. If rubromycosis becomes chronic, the nails and other areas of the dermis remain infected.
Infection on the hands is considered a consequence of self-infection; only in exceptional cases does this pathology act as a primary disease. The clinical picture of rubromycosis of the hands is similar to the signs of foot pathology. There is an intermittent ridge on the periphery of the diseased area of the dermis; it can extend to the palm (back).
Dermatologists most often determine nail rubromycosis if the patient has other dermal diseases. A characteristic feature of the pathology is the simultaneous infection of all nails. White, yellowish stripes appear inside the nail, at its edges.
If the hypertrophic form of the disease develops, thickening of the nail plate, its fragility, crumbling, and the formation of yellow stripes are noted. If the form of the disease is atrophic, the nail becomes thinner, destroyed, and the remains of the nail plate are visible only near the ridge. In some cases, peeling of the nail plate from its bed is noted.
Rubrophytosis of smooth skin in humans (photo)
Generalization
Rubromycosis generalized. Generalization of pathology is carried out for the following reasons:
- trophic changes in the dermis;
- use of medications (antibiotics, cytostatics, hormones);
- diseases of internal organs;
- disorders in the nervous and endocrine system.
Important:
- With the erythematous-squamous form of the disease, unbearable itching appears. Peeling, hyperpigmentation, and an intermittent edematous ridge are observed.
- With the follicular nodular form, deep damage to the dermis is noted on the feet, hands, legs, forearms, and buttocks. Sick areas can merge and grow around the periphery.
With rubromycosis of the body, damage to the intergluteal folds and dermis below the mammary glands is noted. If people are overweight, all the resulting folds will be affected. Lesions have the following external signs:
- infiltration;
- peeling going from the center to the edge;
- intermittent scalloped ridge;
- redness;
- papules, crusts on the cushion.
Causes of rubrophytosis
Fungi of the genus Trichophyton and Dermaphyton, which most often cause this type of inflammation, are highly widespread. They can easily become infected through contact with a carrier of the disease and even a simple handshake. There is a high risk of getting rubromycosis on the leg:
- while visiting public places with high humidity (sauna, bathhouse or swimming pool);
- with a trimmed manicure;
- when using personal belongings, clothing or shoes of a sick person.
The fungus may not manifest itself for a long period of time, becoming more active against the background of exacerbation of chronic inflammation of internal organs. An important role is played by the state of immunity, which can sharply deteriorate due to the use of antibiotics, drug abuse and attacks by pathogenic viruses.
Causes of infection
Infection with rubromycosis occurs due to the influence of factors of exogenous and endogenous origin on the human body.
Exogenous causes that provoke the development of nail and foot fungus:
- Hyperhidrosis as a result of wearing shoes made of synthetic materials that do not allow air to pass through;
- Dry skin of the feet;
- Uncomfortable shoes that contribute to foot injury (formation of calluses, corns, inflammation);
- Lack of foot hygiene;
- Taking antibiotics and antihistamines in large courses;
- Wearing someone else's shoes;
- Use of general hygiene products;
- Failure to comply with personal hygiene rules in public places (swimming pool, sauna, bathhouse, locker rooms of sports institutions, beach and shower cabins).
Endogenous causes of rubromycosis of nails and feet:
- Hormonal imbalance;
- Low immunity;
- The presence of endocrine diseases (problems with the pancreas, diabetes mellitus);
- Diseases of the nervous system;
- Varicose veins of the lower extremities;
- Swelling of the legs;
- Blood diseases;
- Genetic dermatoses;
- Excess body weight;
- Immunodeficiency conditions (HIV, not HIV-related).
Causes of rubromycosis
Diagnostic features
An experienced dermatologist can immediately identify the type of fungal disease during a visual examination. If rubrophytia is suspected on the legs, a scraping is taken from the flaky area, which provides complete information about the type of pathogen and the presence of other viral problems.
Accurate diagnosis is necessary so as not to confuse the fungus with manifestations of psoriasis, seborrheic dermatitis, some forms of eczema, neurodermatitis or dangerous lupus erythematosus. In rare cases, instead of mycotic inflammation, an atypical manifestation of an allergy to chemicals or household drugs may be detected.
Diagnosis of rubromycosis
Skin diseases often raise doubts when trying to identify them with the naked eye. Therefore, only a qualified specialist can determine the cause of the pathology.
Diagnosis of rubrophytosis is carried out on the basis of the clinical picture and the results of a microscopic examination of the affected material:
- nail plate;
- scales;
- vellus hair.
To confirm or refute the diagnosis, doctors additionally conduct research to identify the specific causative agent of the disease - red trichophyton.
A competent specialist can confirm a fungal infection based on external symptoms. To specify drug therapy for a sick patient, mycologists recommend laboratory testing. To study, scrapings are taken from the foot, from under the nails. Cultural culture allows you to determine the type of fungus.
Treatment options
Thermikon ointment for fungus
If the condition is neglected, the skin may become swollen and weepy. In this case, the healing process begins with drying the inflamed areas for further treatment with antifungal drugs.
At the second stage of treatment, after the purulent process has reduced, the dermatologist prescribes special keratolytic compounds. They effectively and easily remove dying epidermis and soften the ridges around areas of inflammation. This is necessary so that the antifungal drugs get closer to the source of colony reproduction.
After cleansing the integument and detaching the dead epidermis, the stage of treating the skin and nails with antimycotics begins. For this purpose, the following medications are recommended:
- Thermikon;
- Terbizil;
- Mifungar.
Treatment for rubromycosis varies in duration and can last up to six months. At the same time, some patients are recommended to use Griseofulvin or Nizoral orally as an antibiotic against a fungal pathogen.
To treat nails with rubrophytosis, it is important to follow a strict diet, the basis of which is proteins and vitamins. To improve the regeneration of the skin and plates, it is recommended to use special mineral complexes and use baths with herbal decoctions.
Before using any medications or traditional therapies, be sure to consult a specialist for advice.
Rubromycosis
The doctor prescribes that areas of skin lesions on the palms and soles should be regularly treated with special exfoliating ointments (for example, Arievich or Whitefield), lubricated with an alcohol solution of iodine 2%, after which, without fail, mycozolon ointments, sulfur ointment 10 or 15% are used, in which the tar concentration should be from 2 to 3%, Wilkinson ointments can also be prescribed. Only a doctor should prescribe treatment after establishing an accurate diagnosis and taking into account the individual course of the disease.
Instead of detachment with ointment, the use of fungicidal-keratolytic varnish may be prescribed. This medicinal varnish must be applied every day to the damaged areas of the foot for three or four days in the form of a shoe. And after completing this procedure, you need to make a special hot bath with the addition of sodium bicarbonate or potassium permanganate in order to completely remove all remaining varnish, as well as the exfoliated stratum corneum.
In the future, all lesions must be lubricated with a 2% iodine solution, and also apply mycozolon ointment or a tar mass of 2 or 3%, which should include sulfur (approximately 10 or 15%), and the use of Wilkinson's ointment may be prescribed.
Thanks to the use of such a medicinal varnish, complete sealing of the affected area is ensured, and a more active effect of all medicinal components included in the drug is stimulated. If children under 7 years of age are being treated, there is a need to halve the concentration of lactic, carboxylic, acetic and salicylic acid, as well as tar and resorcinol.
If the doctor prescribes the use of such varnish for the treatment of this disease, there is no longer a need to re-apply complex gauze dressings, which are very poorly tolerated by children.
In the event that the location of foci of rubrophytosis occurs on the surface of smooth skin or in large folds, in which serious damage to vellus hair begins, the doctor may prescribe the use of sealing the damaged areas with lactic-salicylic-resorcinol collodion or an adhesive plaster.
In the future, the lesions should be lubricated with an alcohol solution of iodine 2%, sulfur 10%, and salicylic ointment 3%. You can replace iodine with canestene, fucarcin, nitrofungin or multifungin.
Simultaneously with the use of external therapy, the doctor prescribes the use of antifungal antibiotics griseofulvin-forte (this is a highly dispersed drug with a high level of absorption in the intestine). Taking into account the patient’s weight, the daily dosage will be calculated - the drug is taken three times a day strictly during meals, and it should be washed down with a small amount of vegetable oil.
During the first two weeks of treatment, this medication must be taken every day, and for the next two weeks every other day, then in the last two weeks of treatment only twice a week. For patients with generalized rubricosis, not only griseofulvin forte is prescribed, but also vitamin A concentrate, which is taken three times a day, 5 or 10 drops (the dosage is determined only by the doctor).
If the patient has a torpid form of the disease, then special biological stimulants can be used for treatment, which include autohemotherapy, pyrogenal, aloe, which increase nonspecific mechanisms of immunogenesis.
Prevention of fungal disease
The process of complete recovery from rubrophytia on the legs is quite long and requires patience from the patient. To reduce the risk of recurrence and development of the fungus, the following rules should be followed:
- do not use other people's shoes;
- maintain hygiene, regularly wash your hands and sanitize your feet;
- monitor your health.
By maintaining immunity at the proper level, you can significantly reduce the risk of infection with the causative agent of this fungal disease.
Symptoms
The symptoms of the disease are as follows:
- Rubromycosis can affect all nails at once, both on the feet and on the hands.
- Infection with the disease most often occurs from the free edge or from the side of the nail plate.
- You may notice that stripes of yellow or white color have formed on the outside of the nail, and sometimes they appear to be visible from the inside.
- At the initial stage of development of the disease, the thickness of the affected nails does not change, but after some time subungual hyperkeratosis occurs, the nails crumble, break and peel.
There is a certain stage of the disease, it is called atrophic, it is characterized by the fact that the nail completely moves away from the nail bed, the plate becomes thinner, and then completely collapses.
Rubrophytia on legs reviews
Pavel, 31 years old
I became infected with rubromycosis this summer when I wore my brother’s slippers to the sea. The brother, in turn, became infected from a friend who foolishly wore someone else’s shoes. I was treated for a very long time, about three months. At first, my mother advised me to make a bath based on potassium permanganate and soak my feet in warm water until it went away. But this method did not give much results. Then I applied Thermikon cream (inexpensive) and after that the fungus began to go away. Your feet itched just terribly, so don’t wear someone else’s shoes and take care of your foot hygiene.
Kristina, 23 years old, Kyiv
My boyfriend had a fungus on his foot - rubromycosis. I was treated with folk remedies for a long time. My feet were soaked in soda, but the effect was short-lived; literally after a couple of days the fungus returned. We bought new shoes, but that didn't help either. On the forum I read about Terbizil 1% cream based on terbinafine. Its qualities are in no way inferior to expensive products like Lamisil, but it costs several times less. I recommend it to everyone.
Dasha, 39 years old
My husband works as a truck driver and is constantly on the road. Of course, there can be no talk of normal hygiene. In general, I contracted rubromycosis somewhere. While my husband was at home, he was treated with everything possible. We bought several creams (Terbinox, Lamisil), smeared them with peroxide, fir oil, steamed them in soda - nothing helped. As a result, my husband developed black spots on his feet. We went to the doctor, and it turned out to be an allergic reaction to all the chemical creams. The doctor forbade me to apply anything and told me to wait. A month later, the spots went away along with the fungus. although they were treated only with propolis. PS Before applying the drug, be sure to consult a doctor so that it doesn’t get worse.
Tatyana Aleksandrovna Pukhova
Dermatologist , 14 years of experience.
Generalist specialist. Engaged in the diagnosis and treatment of diseases of the skin, nails, scalp, as well as sexually transmitted diseases.
Education: 2006 Diploma in General Medicine, Perm State Medical University
Advanced training courses: 2011 “Pillings of superficial-medium impact” 2013 “Plasmolifting in cosmetology and trichology” 2014 “Dermatovenereology”, South Ural State Medical University
Rubrophytia
Zvarych Svetlana Lvovna
Dermatovenerologist.
Rubrophytosis (rubromycosis) is the most common fungal disease of the feet. It affects mainly the feet, and can spread to the hands, large folds, especially the inguinal-femoral folds, and other areas of the skin, often involving vellus and sometimes long hair.
Etiology, pathogenesis. The causative agent is Tr. rubrum. It affects the epidermis, dermis, and sometimes subcutaneous fatty tissue. It can spread not only by continuitatem, but also by lymphohematogenous route. The source is a sick person. For transmission routes, see Athlete's foot. The predisposing factors are the same as for elidermophytosis, as well as a variety of general pathological processes, long-term treatment with antibiotics, corticosteroids and cytostatics, especially in common forms.
Clinical picture. Mostly adults are affected. The most common localization is the feet and hands. The classic form is characterized by hyperemia and dryness of the soles and palms, pronounced thickening of the stratum corneum, mealy peeling, especially along the skin grooves. Subjective sensations are usually absent. Rubromycosis of the feet can also occur as squamous, dyshidrotic and intertriginous epidermophytosis, differing from it in the possibility of affecting the dorsum of the feet, where slightly infiltrated plaques appear, covered with nodules, vesicles, pustules, crusts and scales. Subjectively - itching. Similar forms can be found on the hands, differing here in less intensity. Rubrophytosis of the feet can occur rapidly with general phenomena similar to acute epidermophytosis of Podvysotskaya (see Athlete's foot). Outside the feet and hands, foci of rubrophytosis are characterized by rounded outlines, sharp boundaries, intermittent peripheral ridges, slight infiltration, bluish-pink color with a brownish tint and peeling of varying intensity. Damage to large folds is characterized by powerful infiltration of the skin, numerous excoriations, and painful itching. Manifestations on the legs, thighs and buttocks often occur in the follicular-nodular type. Atypically occurring rubromycosis can simulate a variety of dermatoses: atonic dermatitis, lupus erythematosus, papulonecrotic tuberculosis of the skin, infiltrative-suppurative trichophytosis, staphylococcal sycosis, Dühring's dermatitis and many others. The lesions can be extensive and numerous (generalized form).
The prognosis in the absence of aggravating diseases and proper treatment is good.
Prevention. Personal - prevention of sweating; timely treatment of diaper rash and treatment of microtraumas; correction of circulatory disorders of the lower extremities. Public - fulfillment of sanitary and hygienic requirements in baths, swimming pools, shower facilities and sports clubs.
| Name of service | Price | Special price* |
| Primary appointment with a dermatovenerologist, therapeutic and diagnostic, outpatient | 1,800 rub. | 1,000 rub. |
| Primary appointment with a dermatovenerologist K.M.N., therapeutic and diagnostic, outpatient | 2,100 rub. | |
| Summarizing the examination results and drawing up an individual treatment program, level 2 of complexity | 1,000 rub. | |
| Removal of condylomas on the mucous membrane / for one zone 0.1 cm * 0.1 cm or (1 mm x 1 mm.), for 1 field. | 1,000 rub. | |
| D'Arsonval / face / one procedure | 300 rub. | |
| Wart removal / one piece | 2,500 rub. | |
| Dermatoscopy | 800 rub. | |
| View the entire price list | ||
| *Special prices are not subject to additional promotions and privilege cards. | ||
Causes
What causes rubromycosis? In fact, the cause of infection is the fungus Trichophyton rubrum.
There are many ways of transmitting infection:
- showers;
- baths;
- saunas;
- sports grounds;
- swimming pools.
Dry skin or, conversely, increased sweating, abrasions, and skin cracks are also an increased risk factor for infection.
Can lead to pathology:
- chronic diseases;
- improper blood circulation;
- diabetes;
- immune and metabolic disorders;
- uncontrolled consumption of medications.
Older people are more likely to get this infection. This is expressed by parallel deviations from medical norms in health: weakened immunity and more.