Types of blue tumors
Doctors distinguish 3 main types of blue moles, which can be located on any part of the body:
- Melanocytic nevus, which includes varieties such as pink melanocytic and dysplastic.
- Regular small blue moles.
- Cellular.
Over time, under the influence of unfavorable factors, they can degenerate into malignant neoplasms - melanomas.
All of the listed species can be classified as melanoma-hazardous species. Only ordinary small blue moles are much less likely to degenerate into malignant formations than all other types.
Cellular nevi are characterized by relatively large sizes. Most often, they reach from 1.5 to 3 cm in diameter. The boundaries of the cell-type formation are unclear, often torn. Dark-blue colour. Given these signs, many people mistake a cellular nevus for a malignant neoplasm and immediately begin to panic, which is completely pointless.
Common small blue growths are barely noticeable single formations on the skin. The surface of such a nevus is smooth, the color can vary from light blue to black. As a rule, such a mole is very small, so it does not cause feelings of alarm.
Melanocytic nevus includes several types and subtypes. These are so-called combined formations, which can often degenerate into melanoma. Usually they have signs of both ordinary nevi and cellular nevi.
What is a blue nevus? Is this neoplasm dangerous?
During life, many different neoplasms appear on the body. We can distinguish most of them and classify them as moles, papillomas or warts. But what to do if the neoplasm, at first glance, does not look like anything, and even more so, its color is confusing? Today we will talk about blue nevus, why it appears and whether you should be afraid of it.
What is a blue nevus?
The medical name for blue nevus is Jadassohn-Tiche blue nevus. In fact, this is a benign skin tumor, which is a dense nodule of dark blue or light blue color. The nevus acquires this color due to the accumulation of a large amount of melanin in the deep layers of the skin.
Typically, such a neoplasm has a round or oval shape and reaches sizes from 1 to 3 cm. A blue nevus can rise above the surface of the skin, while having a smooth surface. The color may be uneven, dark blue in the middle and pale blue at the edges. It feels dense and elastic to the touch, there is no pain.
Blue skin nevus can appear at any age. However, most often this occurs during puberty, or under the influence of certain factors:
- unfavorable environment;
- abundant solar radiation;
- serious illnesses;
- viral infections.
A dark blue mole can be found on such parts of the body as: arms and hands, head, face, neck, legs, buttocks. Very rarely appears on the mucous membranes of the mouth, nose or genitals.
Types of blue nevus
Experts distinguish several types of blue nevus:
- A simple blue nevus is a skin growth up to 1 cm, with a smooth surface and a small nodule in the middle. In color, it can vary from light blue to almost black. Most often found on the face, hands, neck, rarely on lymph nodes or mucous membranes.
- Cellular blue nevus can be from 1.5 to 3 cm, has a dark blue color and a rough surface. In most cases, such a tumor appears on the lower back, buttocks and ankle. Due to its external features, it can be confused with a malignant neoplasm.
- Combined nevus - combines the features of the two previous types of blue nevus, its color ranges from light blue to dark blue, most often has jagged edges. This type occurs on the neck and on the back of the hands and feet.
Can a blue nevus become melanoma?
Due to its unusual color and shape, a blue mole on the body can be mistaken for melanoma. You can learn more about what melanoma is in our special article “Skin cancer: melanoma.”
Statistics show that the degeneration of a blue nevus into skin cancer is extremely rare. If you are still worried, then you should carefully examine the nevus; benign neoplasms have:
- uniform color;
- symmetry;
- absence of cracks and hairs;
- absence of pain and itching.
The sudden appearance of a blue mole on the skin can cause understandable concerns. To exclude the possibility of developing melanoma, the neoplasm must be monitored for the first time.
Potentially dangerous nevi grow quickly; their surface begins to peel and bleed; the color uniformity of the neoplasm changes; new nodes and tubercles appear. At the first appearance of one of the listed signs, you should immediately contact an oncologist or dermatologist. And don’t delay – melanoma is a very aggressive pathology with a rapid, often fatal course.
Factors influencing the malignancy of a mole:
- frequent injury to the tumor;
- regular mechanical impact;
- location on an open area of the body;
- decreased immunity;
- hormonal disbalance.
Examination of blue nevus
If the emerging blue nevus causes discomfort and anxiety, it is best to consult a doctor for advice and diagnosis.
The specialist will definitely conduct a visual examination of the neoplasm, noting its shape, color, and structure. For a more accurate diagnosis, dermatoscopy may be prescribed, when the mole is examined under magnification. You can also detect changes in a tumor using RTM diagnostics, which helps to identify even minor deviations from the norm and the development of malignant cells.
Siascopic examination is another method for studying suspicious tumors. It helps to recognize and study the structure of the nevus, as well as the distribution of melanin. For more complex cases, if melanoma is suspected, an ultrasound is prescribed; it shows how deep the nevus is and whether there is growth of malignant cells.
Features of nevi
How to distinguish a blue mole from other neoplasms? It would seem that this is easy to do. But nevi are often mistaken for ordinary, harmless moles. That is why it is advisable to consider the main signs that distinguish a nevus from another neoplasm:
- Most often, a blue mole is colored blue. However, there are often cases when it can have a light blue tint, be gray or black. In any case, such a nevus will not be brown like all the others.
- Often located at a distance from other spots. It is this feature that most characterizes this species. Most often it appears in the buttock area, on the leg or near the lips.
- More than half of blue nevus carriers are women. In men they are much less common. Most often it appears on the body only after puberty. Rarely, such a mole is a congenital formation on the body.
Diagnosis and treatment
It is extremely important to correctly diagnose a blue mole, monitor its condition and know all the main factors that indicate that a skin tumor is beginning to degenerate into melanoma and requires immediate removal. In this case, you need to consult a doctor.
In most cases, experienced specialists diagnose a blue nevus during a visual examination, due to its specific color. But additional examination is still required, especially if there is a risk of degeneration of a benign formation into melanoma.
First, dermatoscopy is prescribed. During the procedure, the nevus is studied in more detail using special instruments. The structure, boundaries, and depth of location of such a mole in the skin are determined. Siascopy helps to further study the structure of the formation and determine the location of melanin in it.
In particularly difficult cases, the doctor can conduct a histological examination and ultrasound of the tumor. This helps to more accurately determine whether the process of degeneration into melanoma has started, or whether it is completely safe. Data from the second type of research show the density of the accumulation of melanocytes, a clearer depth of germination into the skin, and make it clear whether the neoplasm is increasing in size.
Signs that should prompt you to immediately seek help from a specialist are:
- noticeable increase in size of the formation;
- the emergence of new unclear boundaries;
- noticeable change in the shade of the blue mole;
- the appearance of bulges on the neoplasm.
In more severe cases, there may also be a deterioration in general health, increased body temperature and enlarged lymph nodes.
But what to do if a blue mole on the body poses a certain threat to the health and life of the patient? There are many ways to treat blue nevus if necessary. Only a doctor should determine the exact method. Any self-medication can lead to bad consequences.
Most often, blue moles are removed surgically. This is justified in 3 cases:
- If it has already degenerated into melanoma.
- If it increases in size and changes structure.
- If she was seriously injured.
Sometimes neoplasms of this type should not be touched. The verdict is made only by an experienced doctor after careful research. Methods for removing tumors, such as cryodestruction, laser removal and electrocoagulation, are cosmetic. But they also should not be used without a doctor's permission.
Timely detection of such a tumor on your body and its diagnosis can help prevent a life-threatening disease.
After all, theoretically, any mole threatens to degenerate into a cancerous tumor.
Mole blue nevus of the skin: photo and removal, prognosis.
A birthmark located on a person’s skin is called “nevus” in medical practice.
A nevus by its nature is a benign formation that arises as a result of the movement of melanoblasts during the period of intrauterine development.
There are quite a lot of varieties of nevi and they are classified according to groups - melanoma-dangerous and non-dangerous.
It is to the first group that the occurrence of such a formation as a blue nevus, which has another name, is referred to as the blue nevus of Jadasson-Tiche.
Nevus removal methods
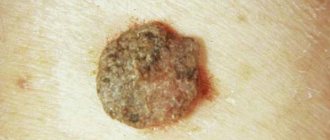
It is believed that blue formations very rarely degenerate into melanoma, but such cases have occurred in medical practice. A sign of malignant melanoma, arising from a blue cellular form, is its rapid increase in size to several centimeters. The surface acquires a characteristic nodular character (photo 4). You should pay attention to the occurrence and manifestation of other typical symptoms:
- pain in the area of the wart;
- change in the color of the nevus;
- the appearance of hair on the mole that is unusual for this form of growth;
- presence of educational trauma;
- enlarged lymph nodes;
- presence of wet discharge on the surface of the stain.
It is advisable to keep the blue growth under constant supervision of a dermatologist, and the carrier of this form of skin disease should strive to prevent possible damage to the hamartoma, so as not to trigger the mechanisms of degeneration of a benign formation and malignant transformation. If these symptoms appear, it is necessary to seek surgical help with a mandatory histological examination of the stain tissue.
The location of the blue nevus in places where there is a danger of mechanical damage, for reasons of a cosmetic nature, is also a reason to contact a specialist and possible removal of the formation: under the nails, on the lymph nodes, or the oral mucosa. They are less common, but may have a tendency to malignancy (degeneration of cells).
Clinical manifestations of blue nevus
Blue nevi are not a risk group for any age category of people, but more often than others they appear during the period of hormonal changes in the body of a teenager.
Mole blue nevus photo
Since the appearance and growth of a blue nevus does not cause a person any discomfort, it is not always possible to immediately recognize its occurrence.
Its localization on the body is typical for the dorsum of the feet and hands, as well as the legs, buttocks, and forearms.
Blue appears extremely rarely on the face.
This formation usually has an oval shape and visually looks like a nodule.
Its contours are clear, but the color of dark blue or light blue is uneven on the surface.
The size of a blue nevus does not exceed 1 cm; a rare exception is a 3-centimeter formation.
In this case, the appearance of the spot may cause the feeling of a foreign body being under the skin.
Causes of blue nevus
Blue nevus is characterized by a large accumulation of melanocytes in the dermis. For this reason, the pigment determines the color of the spots.
The disease occurs in people of all ages, usually during puberty. Thus, blue nevus is not a congenital disease. This type of nevus occurs more often in women than in men. Blue nevus does not cause any pain or discomfort. The formation does not have a specific localization; it can appear on any area of the skin.
The causes of blue nevus have not been clearly identified. At their core, nevi are benign formations that are formed during the migration of melanoblasts (precursors of pigment cells) during intrauterine development. Most likely, the formation of a blue nevus is based on the same factors as in the formation of ordinary birthmarks:
- disruption of the formation of melanocytes, which are responsible for pigmentation in the body;
- changes in the concentration of hormones in the blood of a pregnant woman;
- regular use of contraceptives;
- influence of unfavorable environmental factors (UV radiation, toxic and poisonous substances).
The impact of the above factors on the body of a pregnant woman causes disturbances in the development and localization of melanoblasts (precursors of pigment cells), as a result of which they “clump” into small groups and form a nevus.
Nevi are divided into two large groups:
- melanoma-dangerous nevi;
- harmless nevi.
Melanoma-dangerous nevi are still benign formations that are in a borderline state and require increased attention or drastic therapeutic measures. Blue nevus belongs specifically to the melanoma-dangerous group.
Each nevus has its own specific structure, by which it is recognized and a subsequent strategy of action is developed. Even if a histological examination reveals atypical cells, this does not mean that melanoma is developing. Not all benign tumors become malignant. Atypical cells have signs of a tumor, but this is not always cancer. Degeneration into cancer cells occurs gradually. Initial cell changes before the appearance of malignant symptoms are called precancer.
The melanoma-dangerous group includes: Dubreuil's melanosis, borderline nevus, Ott's nevus, giant pigmented nevus.
The group of harmless nevi includes: Setton's nevus, pigmented fibroepithelial nevus, intradermal nevus, verrucous nevus and verrucous nevus.
Type of blue nevus
Blue nevus can be:
- ordinary;
- cellular;
- combined.
An ordinary nevus has a smooth surface and a dense consistency. The size of an ordinary nevus does not exceed 1 cm; it is usually localized on the hands, body, face and mucous membranes.
Cellular nevus reaches 3-4 cm, has a bumpy surface and a dark blue color. This type of blue nevus is localized only on the body (hands, buttocks, lower back.)
A combined nevus is a cluster of borderline nevi with complex pigmentation and a variety of birthmarks. A cluster of nevi has a lumpy, heterogeneous surface, vague boundaries and strict localization on the lower back, palms, and neck.
Symptoms of the disease
As mentioned above, blue nevus does not cause pain, itching or discomfort to its owner. It can only become a cause of discomfort if its localization contributes to its constant traumatization.
The nevus may rise slightly above the skin or be flat. Sometimes it looks like an infiltrated nodule located under the skin. This location of the nevus creates the impression of a foreign body under the skin. Hair growth is never observed on the surface of the nevus.
Diagnosis of the disease
Diagnosis of the disease is not difficult. Blue nevus is diagnosed by clinical examination. This type of nevus is dangerous because it belongs to the melanoma-dangerous form. Therefore, the dynamics of its development require special attention. You can suspect the degeneration of a blue nevus by the changes that occur to it: a change in color, an increase in size, accelerated growth, uneven borders, and the appearance of discomfort during palpation.
The disease is differentiated from dermofibroma, melanoma and borderline nevus. To accurately diagnose the degeneration of a blue nevus, ultrasound and dermatoscopy of a skin tumor are used. If necessary, surgical removal of the nevus is performed followed by histological examination.
Treatment of blue nevus
Blue nevus usually does not require treatment. You should carefully monitor the condition of moles and undergo periodic examinations by a derma-oncologist. A blue nevus is removed only in cases where it is subject to constant trauma, as this can initiate its malignant transformation. Blue nevus is removed in the following ways:
- cryodestruction with liquid nitrogen;
- laser;
- electrocoagulation;
- radio wave method.
If there are difficulties in differentiating a blue nevus from melanoma, or its pathological changes are noticed, such as: change in color, increase in size, accelerated growth, uneven borders, then the blue nevus is removed using a surgical scalpel. Together with the nevus, an area of healthy skin from 5 to 10 mm and subcutaneous fatty tissue at the location of the nevus are captured. A histological analysis of the removed tissue is required.
Signs of malignant degeneration of blue nevus
You can judge the malignancy of a blue nevus if the following changes are observed:
- increase in size;
- color change;
- lumpy, uneven surface;
- the presence of microcracks and the release of bloody fluid;
- hair growth on nevus;
- discomfort in the area of the nevus.
Causes of blue nevus
Until now, scientists have not clearly formulated the reasons for the occurrence of blue nevus, but the fact that this pigment formation is acquired and not congenital has been established with certainty.
Perhaps the reasons for the appearance of this formation on the body are based on the same factors as a regular birthmark:
- hormonal changes in the body (adolescence, pregnancy, menopause);
- exposure to ultraviolet rays (prolonged exposure to the sun or solarium);
- taking contraceptives;
- allergic or inflammatory diseases of the skin.
Causes of blue nevus formation
A blue nevus is one of the types of birthmarks, so it is formed in a child while still in the womb.
The following are the reasons for the appearance of this mole:
- abnormal fetal development;
- infectious diseases of the genitourinary system of a pregnant woman;
- hormonal imbalances associated with pregnancy;
- the influence of harmful factors, these can be radiation or toxic substances.
In addition, one of the common reasons for the appearance of such a formation is the pathological development or improper placement of melanoblasts.
But a blue mole can increase as a result of the following reasons:
- regular use of hormonal methods of contraception;
- physiological changes in the body - pregnancy, lactation, transition to adolescence;
- various allergic and inflammatory skin diseases;
- the influence of ultraviolet rays - sunbathing at lunchtime, going to the solarium.
Tanning in the middle of the day provokes the growth of moles
Types of blue nevus
Medical practice divides blue nevus into three subtypes:
- Simple - no more than 1 cm, with a smooth surface and dense in consistency. It can appear on the body (usually the hands), face (including the décolleté area) and mucous membranes (uterus, vagina, oral cavity).
- Cellular - can reach sizes up to 3 cm, has a dark blue color with irregularities. For this subspecies, the typical location is only on the body (lumbar region, buttocks, hands and feet).
- Combined - in this case, the blue nevus is combined with other types of dangerous and non-dangerous moles.
What types of blue nevi are there?
- Simple form. This species is characterized by the fact that the shades of such new formations can vary from dark blue to sulfur colors. In addition, the surface of such nevi is disgusting. They are most often found on the neck, arms, face and lips.
- Cellular form. The diameter of such formations can reach 3 cm. Most often, cellular nevi are localized on the hands, lower back and buttocks. Cellular nevi themselves are represented by a collection of large cells. As for the color of such nevi, they have an uneven color. The surface of such moles is rough.
- Combined form. This type of mole consists of an interweaving of blue nevus with other types. In appearance, combined nevi resemble a nodule that is brown and blue in color. Often such moles appear on the lower back, neck, palms, and lips.
It is necessary to emphasize the fact that even after removal, a blue nevus can reappear . As for metastases, they appear very rarely.
Why is blue nevus dangerous?
A formation such as a blue nevus can be a harbinger of melanoma.
Although such cases are extremely rare in medical practice, you should not take this mole lightly.
One of the subspecies of blue nevus can reach up to 3 cm in size.
Signs of a malignant process
A malignant blue nevus will reveal itself with the following changes:
- rapid growth of a blue mole;
- manifestation of pain when pressing on such a formation;
- burning, itching and peeling of the spot;
- change in color tone;
- uneven surface;
- hair growth on a mole;
- discharge of fluid (blood) from the nevus.
Moles of this type that are located on the body in an area with a risk of injury (lumbar region, hands in the cuff area, collar area on the neck, and also on the face) are most susceptible to malignant processes.
Uneven edges of the formation are a reason to consult a doctor for examination.
Types of moles
Today, blue nevus comes in three forms:
- Simple form. Presented in the form of a cluster of cells that are saturated with melanoma. In this case, a nodule protrudes above the skin, measuring no more than one centimeter. The color is variable, from blue to grayish. The surface is smooth. A blue mole of this type is localized in the neck and arms. There are cases when the formation occurs on the face.
- Cellular form. Presented in the form of large accumulated cells, melanoma is much less saturated than in the simple form. In size they can reach about 3 centimeters. The color is uneven and there is no brightness at all. The surface is rough. This type of blue nevus is most often located on the hands, feet, buttocks and lower back.
- Combined form. It is formed as a result of grouping of a blue mole with its other types (for example, intradermal). In appearance, a nevus of this shape is presented in the form of a nodule, the color of which combines brown and blue. The surface is heterogeneous, the edges are unclear. Blue nevus of this form is most often localized in the lumbar region, palms and neck.
The most common is the simple form.
A simple blue mole is a bright nodule protruding above the skin
Treatment and removal of blue nevus
In the case when the blue nevus does not have malignant signs, its treatment is not required.
Treatment by removing the formation is used when the location is inconvenient (which carries a risk of injury) or there is a threat of degeneration of the blue nevus into melanoma.
Such a formation can be treated with various methods depending on its location and size:
- radio wave method;
- cryodestruction;
- laser removal;
- electrocoagulation.
If it is not possible to diagnose a blue nevus (similar to melanoma), then mandatory surgical excision of the formation is required.
In this case, some of the healthy cells under the skin are also removed. After surgery, samples of the formation are sent for histological examination.
Blue nevus of the skin: what is it, photo, removal
Pigment formations are not always brown in color. Sometimes in the practice of dermatologists, blue nevus is encountered. What are its features and what to do when such a mole appears needs to be considered in more detail.
Blue nevus: what is it?
Blue nevus (Jadassohn-Tiche blue nevus) is a small acquired pigmented skin tumor with a characteristic dark blue or light blue color. As a rule, such formations are single, but in some cases multiple blue nevi are also found.
Blue nevus is characterized by a large accumulation of melanocytes in the dermis. For this reason, the pigment determines the color of the spots. The disease occurs in people of all ages, usually during puberty. Thus, blue nevus is not a congenital disease. This type of nevus occurs more often in women than in men. Blue nevus does not cause any pain or discomfort. The formation does not have a specific localization; it can appear on any area of the skin.
Why do blue spots appear?
Many researchers agree that melanocytic nevi appear due to mutations in pigment cells. And they, in turn, can be provoked by various factors:
- Hormonal imbalances.
- Excessive insolation.
- Dermatological pathology.
Against the background of a hereditary predisposition, adverse effects from the outside or from the body itself lead to genetic damage in melanocytes, which becomes a source of tumor growth. This is how blue pigment spots appear.
Blue nevi appear due to genetic damage in melanocytes, which occurs when exposed to external or internal factors.
Classification
Blue nevi come in several types. According to the existing classification, which takes into account morphological and histological features, there are three types of moles:
- Simple.
- Cellular.
- Combined.
The first variety is small in size, has a smooth surface, and is mainly localized on the neck, face and hands. A cellular mole grows up to 3 cm, is dark in color, and lumpy. The combined type is a combination of a blue nevus with an intraepidermal, borderline or complex pigmented nevus.
Classification of blue nevus
Pigmented blue neoplasms come in several types. Taking into account all the morphological and histological features, it is customary to distinguish three forms of blue nevus.
The simple form of the neoplasm is a single node with a smooth surface, the size of which, as a rule, does not exceed 10 mm. It has different colors ranging from black and blue to light gray. A nevus is characterized by an abundance of pigment, which almost completely fills the cells, making it quite difficult to determine the cell nucleus. Often, during microscopic examination, it is discovered that melanin spreads to the walls of blood vessels and nerve endings.
A simple blue nevus on the skin is localized mainly on the face, neck and arms, in rare cases - on the vaginal mucosa and lymph nodes.
The cellular form is represented by the significant size of the mole (from 15 to 30 mm), dark blue color and uneven surface. For this reason, such a nevus is often mistaken for a malignant formation. In most cases, birthmarks are located on the skin of the lumbar region and ankles. Skin cells that produce melanin in this type of neoplasm contain a small amount of pigment, but have signs of division. After the removal procedure, the formation may appear again, but it metastasizes quite rarely.
The combined type is formed due to the grouping of blue nevus with its other types. In appearance, a mole of this shape is represented by a nodule, the color of which is heterogeneous and combines both brown and blue shades. As a rule, the surface of the neoplasm is heterogeneous and the edges are unclear. Most often, a nevus of this shape is localized in the lumbar region and on the back of the arms.
How do they appear on the body?
A blue mole looks like a small (up to 10 mm in diameter) round or oval formation located deep in the skin. This is a nodule of dense consistency with clear edges, slightly protruding above the surface of the skin. The color of the nevus varies from blue to blue-black, its surface is smooth, devoid of hair, but with a preserved epithelial pattern.
The formation can be located on almost any part of the skin, but in half of the cases it is found on the dorsum of the hands and feet. Sometimes it is found on the mucous membrane of the oral cavity (soft and hard palate). Cases of multiple nevus are rarely described, when pigmented formations are located in different parts of the body.
The mole does not bring any subjective sensations and grows slowly, and therefore can remain unnoticed for a long time. Gradually, the blue nevus may become pale and flatten. Very rarely does it degenerate into melanoma, a malignant skin tumor. But even a benign process can be accompanied by the spread of pigment cells to the lymph nodes (cases of familial multiple nevus).
The symptoms of a blue mole are revealed during a medical examination and form the basis of a preliminary conclusion about the nature of the pathology.
Symptoms of blue nevus + photo
In typical cases, a common blue nevus is:
- a slightly raised, symmetrical papule of blue-black color, with a smooth surface, even, but not always clear contours.
- On average, the size of a nevus ranges from 4 mm to 1 cm. It is found mainly on the face, back of the hands and back, in the sacral region, more often in newborns and young children.
- Cellular blue nevi clinically resemble ordinary blue nevi; they often develop at a young age, but can be congenital; they slowly increase in size for some time, can reach several centimeters in diameter, and then remain stable. They often protrude significantly above the surface of the skin.
- Ulceration and bleeding are not typical.
- Preferred localization is the lumbosacral region, head and neck. There are multiple eruptive blue nevi. Rarely, cellular blue nevi can become malignant.
Diagnostics
A typical skin lesion makes it possible to make a correct diagnosis with a high degree of probability. It is based not only on data from a routine examination, but also on the results of additional methods:
- Dermatoscopy.
- Skiascopies.
- Histological analysis.
Tissue examination is performed after the mole is removed. Histological analysis allows us to determine the structure of the tumor and its nature. A simple nevus contains melanocytes with a large number of granules, and in the cellular form they take on large sizes and are depleted in pigment. The tumor is located in the dermis, between the fibers or goes down to the subcutaneous tissue.
Jadasson-Tiche's nevus often requires differential diagnosis. Education must be distinguished from the following states:
- Melanoma.
- Dermatofibroma.
- Venous hemangioma.
Unlike melanoma, a blue mole retains its skin pattern and has clear edges. Dermatofibroma is mainly located in the lower legs and shoulders, and venous hemangioma is soft and turns pale when pressed.
Typical signs of a blue mole
The second name of the neoplasm, Jadassohn-Tiche nevus, is associated with the names of German and Swiss researchers in the first third of the twentieth century, who first described this type of pigment spot and determined its dermal melanocytic origin. The unusual color shades are explained by the high concentration in the deep layers of the dermis of melanocytes - cells that produce melanin, which absorbs the red part of the visible radiation spectrum and reflects the blue. As the number of cells increases, the color of the neoplasm becomes darker. One theory of the origin of melanocytes suggests that they are embryonic neural crest cells that failed to migrate through the epidermis in the usual way.
In simple forms, a blue nevus appears as a collection of cells with a high melanin content and is an oval or round single spot ranging in size from 2 to 15 mm, rising above the skin. The growth has a smooth, glossy surface and is painted in various tones: from gray to blue black. This type of cutaneous hamartoma (benign tumor formation) in almost half of clinical cases is located on the back of the hand, face (photo 1, 2) or in the neck. But medical practice has recorded precedents when a typical form of blue nevus was found on the cervix or vaginal mucosa.
Treatment of a blue mole
If the nevus does not exceed 10 mm in diameter and has a low risk of malignant transformation, then patients are only recommended to undergo regular monitoring by a dermatologist. In other cases, surgical correction is necessary.
How is the removal done?
- Instrumental excision.
- Electrocoagulation.
- Cryodestruction.
- Radio wave method.
- Laser removal.
Surgical tactics are determined based on the characteristics of the pigment formation. If the nevus shows signs of degeneration into melanoma, its wide excision along with subcutaneous tissue and a strip of healthy skin is indicated. In other cases, minimally invasive techniques can be used.
In most cases, blue nevi are removed surgically. The doctor will tell you what is the best way to do this.
What to do if it bursts?
Moles that are traumatized often fill with blood. With further damage, they rupture and burst. In this case, the formation may bleed and be accompanied by pain.
The tactics for providing assistance to a burst mole are simple. It is necessary to treat the damaged area with an antiseptic (hydrogen peroxide) and apply a bandage. To determine further tactics, you should consult a doctor. Most likely, the ruptured nevus will have to be removed.
Blue nevus is a separate type of melanocytic pigment formation. Such a mole is benign in nature, but can undergo malignant transformation. Therefore, blue nevi need to be identified in time and observed by a doctor, and if necessary, do not hesitate with surgical correction.
Synonym
: proliferating blue nevus.
Definition
. A type of blue nevus, characterized by large size and the possibility of transformation into melanoma.
Historical reference
. Cellular blue nevus was first identified as a different formation from melanoma by A. S. Allen in 1949.
Age and gender
. Nevus is congenital or appears in childhood. Diagnosed, as a rule, in children and young people, but sometimes in elderly patients. The average age at diagnosis is 33 years. It is more often observed in females (the ratio of women to men is 2:1).
Rash elements
. The development of a nevus begins with the formation of a spot or compaction in the dermis, which gradually transforms into a node or plaque with a smooth or uneven surface, usually measuring up to 2-2.5 cm in diameter. Some patients may experience mild itching in the area of the nevus. Sometimes the nevus can be large (10 cm or more). It is extremely rare that the tumor may ulcerate. Color blue.
Localization
.
The location of the nevus can be any, but in almost 50% of cases it is located on the buttocks and in the lumbosacral region, less often on the back of the hands and feet. Rare tumor locations have been described: the conjunctiva, scalp, and meninges of the spinal cord. a — Blue cell nevus in the area of the right buttock in a 20-year-old patient.
b — blue cell in the occipital region in a 19-year-old patient. Histology
. It is characterized by large sizes, usually occupying the entire thickness of the reticular layer of the dermis. As a rule, it has a characteristic “hourglass” configuration - it forms limited tumors in the dermis and subcutaneous tissue, connected by a narrow isthmus. The tumor consists of fairly large spindle-shaped cells located in the deep parts of the dermis, forming bundles and swirls. The kernels are juicy, oval or spindle-shaped. The cells are grouped into cells separated by connective tissue layers, in which there are clusters of macrophages with coarse melanin granules. The content of melanin in the melanocytes themselves is variable, from insignificant to abundant. Along the periphery, pigmented melanocytes with long processes are found, indistinguishable from the cells of a common blue nevus. It is believed that the presence of these cells is mandatory for the diagnosis of cellular blue nevus. The absence of borderline activity, epidermal invasion, inflammation and necrosis distinguishes cellular blue nevus from melanoma, as well as the presence of a clear contour, mild cell atypia and the virtual absence of mitoses.
Immunophenotype
. An immunohistochemical study reveals a positive reaction to the markers S-100, HMB-45, Bc1-2 and CD34.
Diagnosis
diagnosed on the basis of clinical and histological signs; it is also necessary to conduct an immunohistochemical study. Difficulties arise in interpreting morphological data.
Differential diagnosis
carried out primarily with melanoma and malignant blue nevus (“blue” melanoma). The microscopic picture of a cellular blue nevus is close in architecture to “blue” melanoma, but it is characterized by pronounced cellular atypia with numerous mitoses and areas of necrosis. The difficulty of diagnosis is evidenced by the following clinical observation.
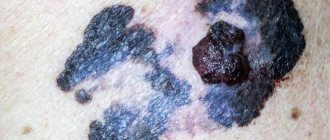
The patient first applied for a pigmented formation on the right buttock at the age of 20. Since birth, she had a bluish formation in this area, which over the past 6 months began to rapidly increase in size and acquired a blackish color. The tumor was excised, the macroscopic picture was a black-gray tumor measuring 1.5 x 2.5 cm, histology was melanoma, level of invasion according to Clark V, tumor thickness was 2.5 cm. Additionally, immunohistochemical and repeated histological studies were performed, which made it possible to establish definitive diagnosis of blue cell nevus.
Course and prognosis
. Currently, depending on the clinical picture, pathomorphological signs, course and prognosis of the tumor process, two forms of blue cell nevus are distinguished: typical (classical) and atypical with uncertain biological potential.
The latter, in its characteristics, occupies an intermediate position between the typical form of the tumor and a malignant blue nevus
(or melanoma arising from a blue cell nevus). Simultaneous damage to different tissues occurs. A case of localization of a nevus in the scalp area with damage to the skin, soft tissues, bones and dura mater in a patient at birth is described. Cases of the development of melanoma against the background of cellular blue nevus have been described.
Malignant transformation
occurs, as a rule, over a long period of time (years) and in people of mature or elderly age and is manifested by a rapid increase in the tumor, its ulceration and color change. Cases of a pigmentless variant of cellular blue nevus have been described. With cellular blue nevus, cells similar to this skin formation may be observed in regional lymph nodes. This process is called “benign metastasis” by some authors.
These changes in the lymph nodes
imitate melanoma metastases, which requires careful differential diagnosis between these processes.
Blue nevus is a common skin disease that belongs to the group of melanoma-dangerous formations. The patient should be thoroughly examined by a dermatologist, since only a specialist can assess the condition of the birthmark.
Blue nevus is one of those pigment spots that need to be regularly examined and their development monitored.
What is a blue nevus
In medicine, a pigmented spot on a patient’s skin is called a “nevus.” Typically, such a formation is benign in nature and manifests itself due to the fact that melanoblasts begin to move in the child’s body even before his birth.
In general, birthmarks can form under the influence of several reasons. Most of the pigmented formations are congenital, including blue nevus. The reasons for its occurrence may be:
- any abnormalities in the genetics of the fetus;
- pathologies in the hormonal system of a pregnant woman;
- some external factors (for example, exposure to radiation or toxic substances).
As a result, melanoblasts begin not only to move, but also to accumulate in a group, which contributes to the appearance of a nevus.
Blue nevus also has another name - “blue nevus of Jadassohn-Tiche.” This pigmented formation on the skin is small in size and has a blue or blue color. Most often, blue nevus is single, but entire clusters of it can also occur.
Blue nevus, under the influence of various factors, can begin to change towards the formation of a malignant tumor. As a result, melanoma develops.
Doctors usually do not seek to remove a blue nevus. The patient is required to regularly undergo diagnostic tests, and only when it is determined that melanoma has occurred, surgery to remove the formation is prescribed.
The occurrence of a blue nevus does not depend on a person’s age, but in most cases its appearance is observed in adolescents during their pubertal development. There are no unpleasant sensations, and, therefore, a person may not notice growth and other changes in education for quite a long time.
By the way, doctors note that blue nevus occurs much more often in women; men are less likely to suffer from this disease.
Blue nevus of the skin: what is it?
Blue nevus is diagnosed in representatives of any age group - from children to the elderly. But most often it occurs during puberty, which suggests the role of sex hormones in the initiation of this cancer.
Blue nevus is less common in men than in women. It has also been noted that it is in males that multiple blue nevi predominate, while in females solitary nevi predominate.
note
White-skinned people get sick more often than dark-skinned people. But it is assumed that in the latter case, the nevus is detected less frequently against the background of dark skin color.
This neoplasm is characterized by slow growth (the neoplasm can increase by several millimeters over several years) or its absence. Since the pathology does not cause any subjective sensations, patients may not even notice it for a long time. There are no exact statistics on incidence, since blue nevus is rarely treated by a dermatologist. In most cases, it turns out to be an accidental medical discovery during preventive examinations or diagnostic examinations for some other dermatological pathologies. Patients also do not always go to the clinic on time if there are changes in the nevus, which may be manifestations of its malignant degeneration.
The pathology has another name - Jadassohn-Tiche blue nevus.
Symptoms of blue nevus
A blue nevus is located under the skin and upon palpation examination is defined as a small nodule of cellular tissue with clear boundaries. Most often this is a round or oval thickening, sometimes taking on a spindle-shaped shape. Blue nevus is 1-3 cm in diameter. The formation can be easily recognized by its blue, dark blue or black-blue color. This color occurs due to the accumulation of a large amount of melanin in certain areas of the skin, in its deep layers.
The surface of the nevus may be uneven, and sometimes hair growth is observed on it. The pigment spot is visually flush with the surface of the skin or slightly protrudes above it. When you press on the formation, a slight compaction of a nodular nature is felt.
Nevus is often localized on the face, forearms, hands or feet, buttocks and legs. There are no painful sensations, itching and burning are not expressed. However, the formation can cause some discomfort if it is located in a place subject to constant friction.
Symptoms and photos of blue nevus
A blue nevus is a nodule with the following characteristics:
- by localization - inside the skin on the back of the feet, hands, legs, forearms, buttocks, less often - on the face and scalp. Nevi are also found in the oral cavity;
- in relation to the surrounding tissues - clearly demarcated, slightly protrudes above the surface of the skin or does not rise above it at all;
- in shape - oval, round or spindle-shaped;
- in size - usually up to 1-3 cm in diameter;
- by color - dark blue, light blue or blue-black. Due to the accumulation of a large amount of melanin in the deep layers of the skin, the color of the nevus may be heterogeneous;
- by the nature of the surface - it is smooth, without hair growth;
- The consistency is densely elastic.
note
Upon examination, a blue nevus resembles a foreign body of the skin.
There are no subjective manifestations of blue nevus (itching, pain, burning). But if it is located in a place that is constantly injured, then a feeling of discomfort may occur.
If the described neoplasm changes, this is a reason to suspect its malignant transformation into melanoma. In this case, the following may occur:
- accelerated growth of nevus;
- change in its color;
- “blurred” contours;
- the appearance of unpleasant sensations.
In dermatology, for convenience, blue nevi are systematized. They are:
- by type - simple and cellular form, as well as combined;
- by quantity – solitary (single) and multiple;
- by localization - intradermal and border.
A simple blue nevus is a single node no more than 1 cm in diameter, having a smooth surface and densely elastic consistency. Its color is typical - from light gray to black-blue. Most often, such a nevus is located on the neck, face and arms. In some cases, it is found on the skin of the torso, oral mucosa, as well as the cervix and vagina.
Cellular blue nevus is larger, from 1.5 to 3 cm in diameter, its surface may be uneven, and its color is often dark blue. These characteristics of a blue nevus make it look like a malignant neoplasm. Most often it is found on the skin of the lumbar region or buttocks, less often on the dorsum of the feet and hands.
A combined nevus is a combination of signs of a simple blue nevus with manifestations of an intradermal or borderline nevus formation.
Diagnosis of blue nevus
There are no difficulties in diagnosing a blue nevus; its external manifestations help: the color of the nevus and the pronounced boundaries of the formation.
Dermoscopy and siascopy allow for in-depth studies. The first procedure reveals the structure of the formation, its possible changes and depth. Using siascopy, the direction in which melanin is located on the damaged area of the skin is determined. Ultrasound is sometimes used to study the growth of the nevus and the risk of its transformation into a malignant neoplasm.
After the nevus has been removed, doctors conduct additional histological examination. It is necessary to identify the concentration of melanin in the deep layers of the skin. Since melanin sometimes accumulates in cellular tissues, these cells become enlarged and group together, leaving connective tissue bridges between the clusters.
Type of blue nevus
Blue nevus can be:
- ordinary;
- cellular;
- combined.
An ordinary nevus has a smooth surface and a dense consistency. The size of an ordinary nevus does not exceed 1 cm; it is usually localized on the hands, body, face and mucous membranes.
Cellular nevus reaches 3-4 cm, has a bumpy surface and a dark blue color. This type of blue nevus is localized only on the body (hands, buttocks, lower back.)
A combined nevus is a cluster of borderline nevi with complex pigmentation and a variety of birthmarks. A cluster of nevi has a lumpy, heterogeneous surface, vague boundaries and strict localization on the lower back, palms, and neck.
- Simple - no more than 1 cm, with a smooth surface and dense in consistency. It can appear on the body (usually the hands), face (including the décolleté area) and mucous membranes (uterus, vagina, oral cavity).
- Cellular - can reach sizes up to 3 cm, has a dark blue color with irregularities. For this subspecies, the typical location is only on the body (lumbar region, buttocks, hands and feet).
- Combined - in this case, the blue nevus is combined with other types of dangerous and non-dangerous moles.
Currently, there are several classifications of moles, distinguishing different types and groups of nevi. Most often in practice
two classifications are used: the first is histological, based on which cells the mole is formed from, and the second divides all nevi into melanoma-hazardous and melanoma-safe. Melanoma-hazardous moles are those that, theoretically, can degenerate into skin cancer.
According to the histological classification, moles are of the following types: 1. Epidermal-melanocytic moles (formed by epidermal cells and melanocytes):
- Borderline nevus;
- Epidermal nevus;
- Intradermal nevus;
- Complex nevus;
- Epithelioid nevus (Spitz nevus, juvenile melanoma);
- Nevus of Setton (halonevus);
- Nevus of balloon-forming cells;
- Papillomatous nevus;
- Fibroepithelial nevus;
- Verrucous nevus (linear, warty);
- Nevus of the sebaceous glands (sebaceous, seborrheic, Jadassohn's nevus).
- Mongolian spots (Genghis Khan spot);
- Nevus Ota;
- Nevus Ito;
- Blue nevus (blue nevus).
- Dysplastic nevus (atypical, Clark's nevus);
- Pink melanocytic nevus.
- Combined nevus;
- Congenital nevus.
Let's look at each type of mole separately.
Borderline nevus
A border nevus is formed from a cluster of cells located at the border of the dermis and epidermis. Outwardly it looks like a flat, slightly raised formation or just a spot on the skin, colored dark brown, dark gray or black.
Sometimes concentric rings are visible on the surface of the nevus, in the area of which the color intensity changes. The size of a borderline nevus is usually small - more than 2 - 3 mm in diameter. This type of mole is prone to degeneration into cancer, so they are considered dangerous.
Epidermal nevus
An epidermal nevus is formed from a cluster of cells located in the superficial layer of the skin (epidermis) and looks like a regular-shaped elevation, colored in various colors, from pinkish to dark brown.
An intradermal nevus is formed from a cluster of cells located in the deep layer of skin (dermis). Externally, the nevus is a hemisphere, slightly rising above the surface of the skin and colored in dark shades - from brown to almost black.
Nevus of the sebaceous glands (sebaceous, seborrheic, Jadassohn's nevus) is a convex flat spot with a rough surface, colored in various shades of brown. Sebaceous nevus forms in children due to disruption of the normal growth of various skin tissues.
Such nevi form during intrauterine development and appear on the baby’s skin 2–3 months after birth. As the child develops, sebaceous nevi grow, increase in size and become more convex.
If a nevus bothers a person from a cosmetic point of view, then it can be easily removed. In this case, it is optimal to remove the mole after the child reaches puberty.
Complex nevus
A complex nevus is a mole consisting of cells of the dermis and epidermis. Externally, a complex nevus looks like a small bump or a group of closely spaced bumps.
Epithelioid nevus (Spitz nevus, juvenile melanoma) is a mole similar in structure to
. Despite the similarity of structure, Spitz nevus is not a melanoma and almost never becomes malignant, but its presence indicates a relatively high risk of skin cancer in a given person.
This type of mole usually appears in children under 10 years of age and grows quite quickly, increasing to 1 cm in diameter within 2 to 4 months. Spitz nevus is a convex formation of red-brown color and rounded shape with a smooth or bumpy surface.
Setton's nevus (halonevus) is a common brown mole surrounded by a wide rim of skin of a lighter shade compared to the color of the rest of the skin surface. Setton's nevi appear in people under 30 years of age.
Over time, such a mole may decrease in size and become lighter in color, or disappear completely. After Setton's nevus disappears, a white spot usually remains in its place, which persists for a long time - several months or even years.
These nevi are safe because they do not develop into cancer. However, people with Setton's nevi on the skin have an increased tendency to autoimmune diseases such as vitiligo, Hashimoto's thyroiditis, etc.
A nevus of balloon-forming cells is a brownish spot or bump with a thin yellow rim. This type of mole very rarely turns into cancer.
Mongolian spot
The Mongolian spot is a single spot or group of spots on the sacrum, buttocks, thighs or back
child. The spot is colored in various shades of blue, has a smooth surface and slightly rises above the skin. The Mongolian spot develops due to the fact that the pigment produced by melanocytes is located in the deep layer of the skin (dermis), and not, as normally, in the epidermis.
Nevus Ota
Nevus of Ota is a single spot or group of small spots on the skin, colored blue. The spots are always located on the skin of the face - around the eyes, on the cheeks or between the nose and upper lip. Nevus of Ota is a precancerous disease because it tends to degenerate into skin cancer.
Nevus Ito
Nevus of Ito looks exactly the same as nevus of Ota, but is localized on the skin of the neck, above the collarbone, on the shoulder blade or in the deltoid muscle area. This type of nevi also refers to precancerous diseases.
Blue nevus (blue nevus) is a type of epidermal mole in which melanocytes produce a blue-black pigment. A nevus appears as a dense nodule, colored in various shades of gray, dark blue or black, and can range in size from 1 to 3 cm in diameter.
Blue nevus is usually located on the dorsum of the hands and feet, on the lower back, sacrum or buttocks. The mole is constantly growing slowly and is prone to degeneration into cancer, therefore it is considered dangerous. Blue nevus should be removed as soon as possible after it is identified.
Dysplastic nevus (atypical, Clark's nevus) is a single spot or a group of closely spaced round or oval spots with jagged edges, colored in light shades of brown, reddish or light red.
In general, moles that have at least one of the following characteristics are considered dysplastic:
- Asymmetry (the mole has unequal contours and structure on different sides of the line drawn through the central part of the formation);
- Rough edges or uneven coloring;
- Size more than 6 mm;
- The mole is not like all the others on the body.
Dysplastic nevi are very similar to melanoma in some characteristics, but they almost never degenerate into cancer. The presence of such dysplastic moles on the human body indicates an increased risk of developing skin cancer.
Papillomatous nevus is a type of ordinary epidermal mole, the surface of which consists of irregularities and outgrowths resembling in appearance
Papillomatous nevus always rises above the surface of the skin and consists of individual tubercles, colored brownish or pinkish and looking very unpleasant. When touched, the mole is soft and painless.
Despite their unsightly appearance, papillomatous nevi are safe because they never develop into skin cancer. However, in appearance, these moles can be confused with malignant skin tumors, therefore, to distinguish such a nevus from cancer, a histological examination of a small piece taken using a biopsy technique should be performed as soon as possible.
Treatment of blue nevus
If transformation of the nevus is not observed and is not predicted, then removal of the formation can be completely avoided. However, the patient is obliged to regularly contact specialists in order to constantly monitor the condition of the pigment spot. The patient himself should be interested in this and carefully monitor the nevus. At the slightest sign of transformation of the birthmark, you should contact a dermatologist.
If the nevus is located in an area of the body that is subject to regular mechanical stress (trauma or friction), the doctor may conclude that removal is necessary. In some cases, such treatment is prescribed to prevent the occurrence of melanoma.
Blue nevus can be removed in several ways: laser or radio wave exposure, electrocoagulation and cryodestruction. The most delicate surgical work is performed in the case of removal of a blue nevus from the face. Surgery is required in cases of suspicion of transformation of a nevus into a malignant formation. The damaged area of skin is deeply excised using subcutaneous tissue. Excision is carried out taking into account the necessary capture of healthy skin around the borders of the nevus in order to avoid the risk of further changes in cellular tissue near the removed formation.
Thanks to timely research, the doctor prescribes adequate treatment to the patient in the early stages. Therefore, a person who has a blue nevus on his body can live a long time and remain almost completely healthy.
Prognosis for blue nevus
The prognosis for blue nevus varies. By itself it does not pose a danger. But the possibility of degeneration into a malignant tumor does not allow us to determine the prognosis for this disease as favorable.
When the blue nevus is removed, the prognosis improves.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
6, total, today
( 62 votes, average: 4.42 out of 5)
Dermatoses: causes, symptoms, treatment
Bullous pemphigoid: what it is, symptoms and treatment