Melanoma is a malignant neoplasm that develops as a result of neoplastic transformation of melanocytes. The localization of the primary tumor process can be not only in the skin, but also in the mucous membranes of the digestive system, genital tract, choroid and other tissues.
Melanoma metastasis in the sentinel lymph node 3.1 mm
With melanoma, as well as with other types of malignant neoplasms, there is a high probability of metastatic damage to regional lymph nodes and other organs. Metastasis is a distant tumor site that originates from atypical cells of the primary site. Metastasis in melanoma is common, and in some cases, the growth of metastases is detected earlier than its original source.
Principle and routes of metastasis
The process of the appearance of secondary foci of neoplasms is very complex and has not been fully studied. It is assumed that the cause of metastasis is a disruption in the interaction between atypical cells of the primary tumor, the extracellular matrix and normal cells. Several proteolytic enzymes have been discovered that trigger the degradation of the extracellular matrix and improve the adhesion of cancer cells, which allows them to move throughout the body and invade any tissue. Vascular endothelial growth factor plays an important role in the growth of secondary tumors, which stimulates the formation of new vessels, which subsequently feed the tumor. The spread of melanoma metastases usually occurs through the lymphatic and blood vessels. Most often, secondary lesions appear in the lymph nodes, skin and subcutaneous tissue, bones, liver, lungs, and brain.
How does melanoma metastasize?
Midkine protein secreted by melanoma creates niches for metastases
Vyacheslav Kalinin, “Elements”
Rice. 1. General diagram of the path along which melanoma forms metastases in distant lymph nodes and organs. Contrary to previously accepted views, this process does not involve the formation of lymphatic vessels in and around the primary tumor. growth factor (MDK), produced by tumors, is secreted in free form and as part of exosomes . It reaches distant pre-metastatic lymph nodes and organs, in which metastases will then form. Whether midkine circulates in the lymph and/or blood remains unknown. Midkine induces lymphangiogenesis at these sites, which helps prepare them for the arrival of cancer cells. Drawing from a popular synopsis for the discussed article in Nature
Lines of laboratory mice have been constructed that make it possible to trace the formation of new lymphatic vessels throughout the body. The cell growth factor midkine, secreted by melanoma, has been shown to stimulate this process and prepare niches for the formation of metastases far from the tumor. The findings may allow the development of new markers to determine the risk of metastasis, as well as new approaches to prevent and treat metastases.
Cancer as a cause of death is confidently taking first place in the world, and in a number of developed countries it has already taken this position. The primary cancerous tumor is not as dangerous and can often be removed surgically. Much more dangerous are cancer cells that spread throughout the body and can develop into secondary tumors (metastases), sometimes even in organs and tissues very distant from the primary tumor. Active research is underway to determine the pathways of cancer cell migration throughout the body and block the formation of metastases. These problems have not yet been solved, and any noticeable step in resolving them is very important both from the point of view of theoretical and practical oncology.
Cutaneous melanoma is a common, aggressive disease with very early colonization of lymph nodes by cancer cells, preceded by active formation of new lymphatic vessels (lymphangiogenesis). Removing the primary tumor and nearby lymph nodes does not always prolong the patient’s life. Moreover, as melanoma progresses, the lymphatic vessels of the tumor collapse and lose their function. Therefore, it remained unclear whether and how lymphangiogenesis is associated with melanoma metastasis. It has been suggested that proteins secreted by the tumor and/or its stroma are associated with the formation of niches for metastatic melanoma cells. Studying the role of lymphangiogenesis in melanoma and other malignant tumors has been hampered by the lack of suitable experimental animals for imaging distant pre-metastatic niches.
Scientists led by María S. Soengas from the Spanish National Cancer Research Center, together with colleagues from several other medical and scientific institutions in Spain and the United States, focused on tracking lymphangiogenesis throughout the body. To do this, they took advantage of the known property of vascular endothelial growth factor receptor 3 (VEGFR3). Its expression in the cells of lymphatic vessels is normally strongly suppressed, but it is sharply activated under pathological conditions, during inflammation and cancer. Using genetic engineering methods, the authors constructed lines of model mice in which the gene for the fluorescent protein luciferase was placed under the control of the Vegfr3 promoter.
Using a sensor that records fluorescence, they observed the growth of lymphatic vessels throughout the mouse body after transplantation of cultured melanoma cells under the skin, depending on the progression of metastasis (Fig. 2).
Rice. 2. Luciferase emission after transplantation of melanoma cells into mice. On the left are shown mice after transplantation of melanoma cell lines with less potential for metastasis, on the right – with greater potential. The numbers in the photo are days after implantation. Primary tumors are outlined in red dotted lines. Figure from the discussed article in Nature
It turned out that the growth of blood vessels in various parts of the body distant from the transplantation site occurs regardless of their growth around the primary tumor. Therefore, lymphangiogenesis around the primary tumor does not determine metastatic colonization of cancer cells in other organs and tissues. Moreover, tumor expression levels of vascular endothelial growth factor C (VEGFC), which binds to and activates VEGFR3, did not correlate with the formation of distant metastases. That is, lymphangiogenesis in distant areas of the body is not associated with the production of VEGFC by the tumor.
It has previously been shown that tumors induce the formation of niches for metastases in distant organs before metastatic cells arrive there. If the tumor is removed, metastases can still form in these niches. The authors showed that even poorly developed tumors induced luciferase expression in the lymph nodes of the liver, spleen and lungs. After some time, metastases formed there. Removal of the tumor was accompanied by a significant decrease in the level of luciferase in pre-metastatic areas, but later it could increase again, and subsequently metastases formed there (Fig. 3).
Rice. 3. Quantitative assessment of luciferase emission after transplantation of melanoma cells into mice and removal of the primary tumor (blue numbers indicate the moments: 1 – tumor implantation, 2 – before removal of the primary tumor, 3 – after removal, 4 – after detection of metastases). Data are shown for lymph node, lung, and skin metastases. Figure from the discussed article in Nature
These data indicate that activation of distal lymphangiogenesis induced by tumor cells is an indicator of the formation of a pre-metastatic niche.
Since VEGFC was found not to be the cause of distant lymphangiogenesis and metastasis, the authors investigated other tumor-secreted factors that could be associated with these processes. Using liquid chromatography and mass spectrometry, they compared sets of peptides resulting from the breakdown of proteins secreted by cultures of melanoma cells with different abilities to form metastases. Comparison with catalogs of “peptide signatures” showed that the most likely candidate for the role of an inducer of lymphangiogenesis is midkine (MDK). This small protein is known as a cell growth factor, specifically stimulating blood vessel growth, but its involvement in lymphangiogenesis was not previously known.
Immunohistological analysis showed that midkine is actively produced by melanoma cells with a high potential for the formation of metastases, and very weakly in cells with a low potential (Fig. 4).
Rice. 4. From left to right, histological preparations of melanoma cells transplanted into mice with an increasing potential for metastasis are shown. Midkin is visible as red streaks and spots. Figure from the discussed article in Nature
Suppression of midkine expression and secretion using a specifically selected hairpin RNA (shRNA) did not affect the expression of VEGFC or VEGFD. Moreover, it did not affect the growth of blood vessels in xenograft (caused by human melanoma cells) tumors. But the formation of lymphatic vessels in them was suppressed. The most striking effect of midkine suppression is the cessation of luminescence and the formation of metastases in distant lymph nodes and organs (Fig. 5). In mice with suppressed midkine expression, no metastases formed at all after removal of the primary tumor. At the same time, increased expression of midkine, induced by the introduction into cells of a lentiviral vector carrying the encoding midkine gene, transformed cells with a weak potential for metastasis into actively metastasizing ones.
Rice. 5. Left: Luciferase emission (color indicates intensity) after mouse transplantation of melanoma cells. The use of special “hairpin” RNAs that turn off the gene encoding midkine suppress lymphangiogenesis (the results of using two of the five such RNAs used in the work are shown). Figure from the discussed article in Nature
The culture medium of cells actively secreting midkine stimulated the proliferation of the endothelium of lymphatic vessels. And in the mouse body, midkine accumulated in the developing lymphatic vessels (Fig. 6). This led to the activation of the mTOR protein in the endothelium, which stimulates proliferation. In addition, midkine not only stimulated lymphangiogenesis, but as such promoted the adhesion of cancer cells in newly formed lymphatic vessels.
Rice. 6. Midkin (green) accumulates in places where new lymphatic vessels form and enter the lymph nodes (shown by arrows). Asterisks indicate stromal cells. Lymphatic vessels are contrasted in red. Figure from the discussed article in Nature
In summary, these studies have uncovered the mechanisms by which midkine-secreting primary melanoma tumors induce lymphatic vessel growth. This, in turn, leads to the formation of pre-metastatic niches through still unknown processes.
A retrospective study of benign moles and human melanoma also showed an association of midkine expression with clinical disease. For operated patients who had a high level of midkine in tumor-free lymph nodes, the prognosis for relapse-free survival was significantly worse than for patients with a low level of midkine.
The results of the work discussed are of great importance for both theoretical and practical oncology. But a number of important questions remain unanswered. In what ways does midkine reach distant parts of the body through blood and/or lymphatic vessels? Which receptor of endothelial cells of lymphatic vessels is associated with lymphangiogenesis? To what extent can the results obtained in melanoma be generalized to other cancers?
From a practical point of view, midkine and lymphangiogenesis can serve as good molecular and functional markers of metastasis risk. Lymphangiogenesis and its drivers (midkine, mTOR and others) may become targets for new methods and means of preventing metastasis.
Sources: 1) D. Olmeda et al. Whole-body imaging of lymphovascular niches identifies pre-metastatic roles of midkine // Nature. 2020. V. 546. P. 676–680. 2) A. Hoshino, D. Lyden. Metastasis: Lymphatic detours for cancer // Nature. 2020. V. 546. P. 609–610. (Popular synopsis for the article under discussion.)
Portal “Eternal Youth” https://vechnayamolodost.ru 09/01/2017
Melanoma metastases in the brain
The first signs of brain damage are neurological disorders, which can be represented by different symptom complexes:
- Focal and general cerebral symptoms, which typically have a gradual onset and a long course over several weeks.
- Symptoms that mimic a stroke. They develop as a result of hemorrhage in metastatic tissue or when a blood vessel is blocked by a metastatic embolus.
- Symptoms that mimic brain inflammation and vascular damage.
In practice, a combination of general cerebral and focal symptoms is most often observed. Patients complain of headaches, nausea and vomiting, dizziness, impaired motor and cognitive functions, convulsions, and changes in vision. In severe cases, high intracranial pressure develops, which can cause compression of the brain and wedging it into the foramen magnum, which often leads to the death of the patient.
Magnetic resonance imaging with contrast is the most informative in diagnosing brain metastases, which allows you to visualize brain structures and detect affected areas. In all cases, it is recommended to perform an electroencephalogram to detect seizure activity. Additionally, an examination by an ophthalmologist is prescribed to diagnose changes in the fundus.
Methods of treatment of secondary foci of oncology in the lungs
An oncologist and a specialist will prescribe a comprehensive treatment consisting of several approaches, including:
- surgical excision;
- targeted therapy;
- radiotherapy;
- immunotherapy;
- radiofrequency ablation.
Additionally, symptomatic treatment is prescribed to alleviate the condition and improve the quality of life.
The prognosis for melanoma with metastases in the lymph nodes depends on the number of affected areas. If 1 lymph node is affected, the survival rate reaches 50 percent. If 2 or more lymph nodes are affected - 15-25%.
At the fourth stage, the prognosis is more favorable if only the lymph nodes are affected without the appearance of metastases in the internal organs. The survival rate in this case is 5%.
Such data were obtained based on the results of five-year survival. Statistics do not take into account the specific course of the disease in different patients or the success of the chosen treatment tactics. The sooner metastases in melanoma are detected and removed, the more favorable the prognosis.
List of sources:
- Marochko A. Yu. et al. Melanoma metastases without an identified primary focus // Far Eastern Medical Journal. – 2009. – No. 1.
- Aliev M.D. et al. Modern approaches to surgical treatment of metastases of malignant tumors in the bones // Problems of tuberculosis. – 2001. – T. 2. – No. 1. – pp. 39-43.
- Pak D. D., Lazutina T. N. Determination of sentinel lymph nodes in the treatment of patients with skin melanoma // Siberian Journal of Oncology. – 2008. – No. 1.
- Kallistov V. E. et al. Surgical treatment of bone metastases // Bulletin of the Russian Cancer Research Center named after. N.N. Blokhin RAMS. – 2003. – T. 14. – No. 2-1.
There are no similar articles.
In modern medicine, the following methods are used to treat metastases in the lungs:
- Surgical intervention - the affected area is removed. This method of treatment is effective only if there is a single focal lesion, so it is used quite rarely;
- Chemotherapy is an addition to other treatment methods. The duration of the chemotherapy course depends on the main method of treatment and the patient’s well-being. In medical practice, chemotherapy is used in conjunction with radiation therapy. To raise the level of leukocytes in the blood after the procedure, dexamethasone is prescribed;
- Radiation therapy helps slow down the active growth of cancer cells and reduces pain. Irradiation is carried out in stationary conditions using a remote method;
- Hormonal therapy - used in the presence of a hormone-sensitive primary lesion in the prostate or mammary glands. Serves as an addition to primary therapy;
- Radiosurgery - a procedure that allows you to remove hard-to-reach tumors using a cyber-knife (beam of rays).
Treatment of secondary oncology in the lung can also be done using traditional methods. The most common folk remedy is celandine. It is necessary to pour boiling water over a tablespoon of dried herb and leave in a thermos for about an hour and a half. Then strain the infusion and take it twice a day, two tablespoons before meals.
In conclusion, we can say that there are various forms of lung cancer. This includes both primary cancer and metastases that have spread from other foci. The disease can be asymptomatic, which means that the patient can seek help when treatment no longer gives the desired result.
Until recently, the presence of metastases sounded like a death sentence. There was practically no possibility of surviving after a debilitating course of chemotherapy. Cytostatics, drugs for inhibiting cell division, opened a second front, finishing off the exhausted body with side effects. The main ones: a destructive effect on the bone marrow, irreversible processes in the liver and, as an option, lethal changes in blood composition.
The operations did not give the expected result: after radical removal of the affected tissue, a non-viable organ was often left.
“Doctor, how long do I have left?” – oncologists have to answer a well-known sad question almost every day, sometimes multiple times. It is difficult to predict life expectancy. How long a patient has to live depends on a number of factors:
- where is the primary malignancy located?
- physical condition of the sick person;
- number of years lived by the patient;
- the presence of metastases to organs other than the lung, etc.
The determining factor has not yet been named: at what point in the development of the tumor the patient sounded the alarm and consulted a doctor.
Metastases in the lungs
Metastases in the lungs are sad evidence that the body’s resistance forces have been exhausted, and the cancer cell rushes unhindered through the bloodstream. Medicine today is not always able to cure a patient - to completely cope with metastases. The prognosis for such a diagnosis is often unpleasant due to the lack of obvious symptoms at the beginning of the process.
Positive prognosis is provided by timely treatment of the primary tumor. People sometimes live relatively long after operations associated with metastases that recur a year later.
We suggest that you familiarize yourself with the Causes of melanoma on the face
Good results were obtained when primary tumor foci were found in the body of the uterus, breast, bones, liver and soft tissues.
The location of the secondary cancer: central or peripheral does not significantly affect survival. Life time does not depend on the side of the organ affected by cancer, or on the presence of metastases in the pleura.
The neoplasm, which qualifies as highly differentiated, is encouraging with optimistic forecasts. Such cancer cells resemble healthy ones and spread slowly. In the latter case, the tumor is treatable. Early detected pathology prolongs life up to 5 years.
If a poorly differentiated tumor is not treated, the patient can live 100 days. Cells of this type of tumor are extremely aggressive, but sensitive to chemotherapy and ionized radiation. Seventy percent of patients continue to live if therapy is carried out in a timely manner; the malignant process is detected at a maximum of the second stage of development.
In addition to the fact that the determining factor in the metastasis of tumors of various organs specifically to the lung are multiple blood vessels of the lung tissue, in some cases the situation is also facilitated by the close relative position of a number of organs.
Lungs' cancer
The course of the treatment algorithm is determined by the type of initial tumor formation and the tumor’s response to therapy. The course of action depends on the patient’s condition and whether metastases are detected in other organs.
Chemotherapy
Oncology treatment comes down to destroying cancer cells and preventing their spread. The main method is chemotherapy - the introduction of antineoplastic substances through the blood and stomach. They are treated with chemotherapy alone and in combination with other methods.
According to the tasks to be solved they are classified:
- Adjuvant (remaining fragments of tumors and relapses of metastases are excluded);
- Neoadjuvant (the size of the tumor is reduced and the degree of cell acceptance to drugs is determined);
- Therapeutic (reduction in the size of the secondary tumor, general improvement in the patient’s well-being).
Radiation therapy
The purpose of ionized radiation is to apply high doses to the tumor locally, minimally affecting other tissues. To do this, it is necessary to identify exactly where the malignant formation is located in order to correctly determine the direction and depth of irradiation.
If the lung is damaged due to the dissemination of hormone-dependent neoplasms (breast cancer, prostate cancer), treatment with medications is prescribed. Such therapy is not carried out separately, but in combination with other types of treatment.
Radiosurgery
The method is indicated for people if open surgery is accompanied by risk. The patient is exposed to high doses of radiation. When the tumor is located in places difficult to reach with a scalpel or near vital organs.
Surgery is indicated if:
- there is no initial focus of cancer or relapse;
- no metastases to other parts of the body;
- no more than three foci of metastases in the lung;
- after initial treatment, tumors do not appear within a year;
- the time interval between the first and second metastases is at least six months;
- the patient will be able to tolerate prolonged exposure to anesthesia.
The size of the tumor determines the extent of the operation. Surgical intervention can be aimed at excision of a fragment of the lung - lobectomy, or complete removal of the organ - pneumonectomy. The radical method increases the survival rate for lung cancer.
Brachytherapy
This type of contact radiotherapy involves placing a radioactive implant directly in the bronchi.
This type of therapy is used when all possibilities for radical treatment of the patient have been exhausted, but it is possible to relieve pain syndromes and at least reduce the symptoms of the disease and slow down the process.
The part of the lung affected by the tumor does not participate in the breathing process; the entire load is placed on the remaining healthy tissue and the paired organ. But gradually the tumor stops responding to treatment and replaces large volumes. The patient begins to experience difficulty breathing and oxygen deficiency develops. All organs, especially blood vessels and the heart, experience a lack of oxygen.
Symptoms of oxygen starvation are manifested by:
- Initially, shortness of breath occurs when walking and after physical exertion.
- Later, these symptoms bother you even with minor exertion.
- In a serious condition, a person experiences constant suffocation, a painful cough, rapid heartbeat, weakness, and swelling.
- Any movement aggravates the situation.
The lack of oxygen is compensated by oxygen therapy. The duration of the session is fifteen hours daily. Such treatment is carried out in palliative medicine departments or hospice.
In severe cases, oxygen therapy alone is not enough; artificial ventilation of the respiratory system is needed. Such assistance can alleviate the severity of the patient’s condition:
- make breathing easier;
- temporarily relieve the respiratory muscle from stress;
- replenish oxygen in the blood;
- reduce inflammation temporarily;
- provide psychological support.
Melanoma metastases in the skin
Foci of secondary tumors in the skin and subcutaneous tissue occur in an average of 15% of cases. The development of skin metastases depends, first of all, on the size of the primary tumor, its location, the patient’s age and other characteristics. The routes of spread of melanoma metastases to the skin can be both lymphogenous and hematogenous.
There are several forms of secondary tumor foci: satellite, thromboembolic, nodular, erysipelas. Melanoma is characterized by single and multiple metastases, which are located both near the primary site and far from it. Color, size, shape and consistency can vary. Due to such varied clinical presentations, differential diagnosis is often required.
Causes of metastasis
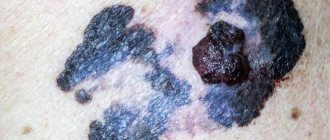
Melanoma is the uncontrolled malignant division of skin tumor cells. The higher the stage, the deeper and more widespread the tumor is. Examples of describing a tumor by stage:
- zero – the appearance of a small mole of rich black color, sometimes red-brown;
- the first – sizes up to 1 millimeter, without pain or discomfort; more about stage 1 melanoma→
- the second – sizes up to 2 millimeters, germination begins up to 4 mm deep, ulcers may appear on the surface, asymmetrical, has radial growths to the sides; more about stage 2 melanoma→
- third - a noticeable increase in the size and depth of germination, the nearest lymph nodes and soft tissues are affected, the surface of the lesion is covered with ulcers;
- fourth - extensive damage not only to nearby tissues, but also to other organs; skin melanoma metastasizes to the liver, brain, and lungs. Read more about stage four melanoma→
The likelihood of metastasis is greatest when the thickness of the lesion is more than 4 mm. The cause of melanoma metastases to the lymph nodes and nearby soft tissues is the spread of malignant cells. They move with the lymph flow - it is for this reason that metastatic melanoma primarily affects the nearest lymph nodes.
The more advanced the stage, the more cells with the lymph flow penetrate into the soft tissues and organs found along the path of the lymphatic flow. The first barrier to this current is the lymph nodes. At this time, metastases can still be removed.
From the fourth stage, metastatic melanoma spreads to the following organs:
- skin – 58% of cases;
- lungs and bronchi – 35%;
- liver – 30%;
- brain – 20%;
- bone tissue – 17%;
- stomach and intestines – 10%.
Damage to each of these organs is accompanied by typical symptoms. But these symptoms are not always caused only by melanoma metastasis. It is always better to consult a doctor immediately to determine the root cause and begin treatment on time.
Metastases, although they are secondary foci, in fact represent a separate tumor in another part of the body. In other words, metastases are also tumors, multiple, although smaller in size than the original cause.
The danger is that the spread of malignant cells and their removal from distant areas is significantly more difficult. It all depends on the specific subtype and stage of melanoma, but the larger the metastasis, the more difficult it is to treat the pathology.
Organs and their systems are interconnected. In addition to the danger that metastases will not be removed and will continue to grow, there is a risk of disorders due to functional abnormalities of the affected organs.
Diagnosis and treatment of melanoma metastases
Scientists classify melanoma as one of the most malignant and aggressive tumors, because... it tends to spread quickly throughout the body. Therefore, when it is detected, additional studies are immediately carried out to identify metastases. At the outpatient stage the following are prescribed:
- Computed tomography of the chest organs.
- Computed tomography of the abdominal cavity and pelvic organs with contrast.
- Bone scintigraphy.
- Ultrasound of regional lymph nodes and internal organs.
- MRI of the brain.
- Determination of protein S-100, a high level of which is characteristic of disseminated tumor processes.
Timely detection of metastases at an early stage of diagnosis can improve the prognosis for the course of the disease and determine treatment tactics.
Metastatic melanoma is treated in a combination way. Usually they resort to surgical removal of the primary tumor and regional lymph nodes, followed by conservative treatment. Radiation therapy is used for secondary brain damage.
Removal of stage 0 skin melanoma can be performed on an outpatient basis. In stage I of the disease, organ-preserving surgery or wide excision of the primary lesion with removal of lymph nodes is performed. At stages II and III, the primary tumor and lymph nodes are removed, and drug therapy is prescribed. In stage IV with distant metastases in any organ, treatment is individual and depends on the patient’s condition. Radiation, immunotherapy, and surgical interventions are used. Alternative surgical techniques, such as radiofrequency ablation, can be used to remove solitary lesions in the liver.
Forecast
Melanoma with metastases is a fairly serious diagnosis. In the presence of a secondary lesion in one organ, the average five-year survival rate after successful treatment is 15-20%, and ten-year survival rate does not exceed 15%.
Skin cancer metastases have a high risk of recurrence. As a rule, the reappearance of secondary lesions occurs within 3-5 years after the end of treatment, especially often in patients from risk groups (dangerous localization, size of tumors, old age of the patient, etc.). If you have a history of melanoma, you should visit an oncologist once a quarter.
Despite the high aggressiveness of the disease, a diagnosis of skin cancer is not a death sentence. The chances of a long life after therapy depend not only on the effectiveness of the chosen course and the stage of the disease, but also on the state of the body and spirit of the patient himself.
5 years - 43%;
10 ‒ 35%;
15 ‒ 28%;
20 ‒ 23%.
Prognostic 5-year results for people under 50 years of age with regional distribution are higher. They indicate a 48% survival rate. For females the chances are higher than for males: 49% to 40%.
According to the data, 4 out of 10 people (40%) who used surgical resection for metastatic tumors are alive after 5 years. Relapses are observed in only 34% of patients.
Depending on the number of nodes affected, the 5-year life expectancy ranges from 53% (for a single metastasis) to 25% (for 4 or more).
The average survival rate for stage IV metastatic cancer is 6-10 months.
When the disease has progressed to the level of melanoma - metastases to the lymph nodes, it is necessary to carefully and adequately evaluate all possible treatment methods, since effective therapy can significantly increase the chances of long-term survival and prolong the patient’s life.
In cases where melanoma metastases have spread to the lymph nodes, the prognosis for five-year survival is about 45%, provided that surgery has been performed to remove them. The younger the patient, the greater his chances of recovery.
Approximately 40% of patients live longer than 5 years after removal of the primary lesion and affected lymph nodes. Unfortunately, with metastasis to internal organs, the prognosis is not good, and in this case, treatment is aimed at alleviating the symptoms of the disease.
In any case, with such a diagnosis as melanoma with metastases, it is necessary to fight, only those who do not give up win. There are cases where people overcame the disease and lived a healthy and happy life.
In summary, it should be noted that melanoma is an extremely serious disease, which one should not be afraid of, but rather try to overcome in every possible way.
You should not wait until metastases form; it is necessary to begin treatment at the first manifestations of the disease. Treatment should be carried out only in qualified institutions and under no circumstances self-medicate.
The location of melanoma metastases and the number of affected areas are quite important. According to the results obtained during a survey of 200 patients with melanoma at stage 4 cancer.
in 59%, the skin, subcutaneous tissue and distant lymph nodes were primarily affected. The average life expectancy in such patients was about 7 months, and in only 25% of patients it reached 1.5 - 2 years.
To a lesser extent, secondary tumors affected the lungs, brain, bones and liver. In this case, the life expectancy of patients with melanoma metastases ranged from 3 to 7 months, and only 8–10% of them were able to live for more than a year.
Moreover, it is worth noting that survival rates do not depend on whether the patient had one affected area or two distant ones at once. Patients with melanoma metastases in one area lived up to a year in 36% of cases, with 2 - in 13%, and in more than three affected areas, no more than a year.
With metastasis, the prognosis is disappointing. Patient survival is low. Metastasis at stage 4 can go to the brain and other internal organs. Mortality in this case occurs approximately after a year. If surgery and individual therapy are performed, the prognosis may improve.
Which organs are susceptible to metastasis?
One of the aggressive and fast-growing types of cancer.
Typically, a cancerous tumor metastasizes to the lymph nodes. More often the pathology is observed in men. If the melanoma is thinner than 0.75 mm, the likelihood of metastasis is low. If the tumor thickness is 4 mm, lymph node involvement is diagnosed in 60% of cases. Cancer cells spread throughout the body through the bloodstream less often than the lymph nodes are affected.
According to medical statistics, skin cancer metastasizes the following organs and tissues:
- Lymph nodes, skin, subcutaneous tissue. It is most often affected.
- Lungs. The probability of metastasis penetration is 25%.
- The liver and bones are affected in 17% of cases.
- Brain. The probability of metastasis is 16%.
Prognosis for metastasis
Metastatic melanoma appears due to the following reasons:
- Female. In women, the incidence is 0.5 times higher. This is due to chromosomal and genetic characteristics.
- Age over 70 years. Elderly people accumulate a large number of gene defects.
- Hair color. Blondes and red-haired people are more likely to suffer from such complications. They have no protective pigment.
- Eye coloring. Those at risk include those with blue, green or gray irises. In such people, protective pigments are in low concentrations.
- The presence of freckles on the face.
- A large number of moles. They are the ones who degenerate and metastasize.
- Congenital pigment spots. They are called nevi. These spots often give rise to areas of metastasis.
- Injury to all kinds of skin formations. This especially applies to those structures that rise above the skin. Patients touch them when going to the shower or getting dressed.
- Age spots. These rashes can also degenerate and metastasize.
- Xeroderma pigmentosum. It is a genetically determined systemic disease.
- Sun or thermal burns. With such trauma to the skin, irreversible changes in the structure of the dermis occur.
- Melanoma spreads deeper than the basal layer. When a tumor penetrates into deep tissues, it is a guarantee that metastases will spread throughout the body by hematogenous and lymphogenous routes.
Metastases in melanoma are evidence of its progression. Accordingly, they are considered a poor prognostic sign. But if metastasis is detected in a timely manner and drug measures are started immediately, the prognosis for life and recovery improves. The survival rate of well-treated patients with this diagnosis is 85-90%.
The spread of melanoma cells to the liver leads to the formation of metastases. Changes are happening quite quickly. Secondary liver damage can be represented by a single metastatic focus, as well as multiple disseminated forms. Clinical manifestations of melanoma metastases to the liver will depend on the volume and location of the process. Symptoms are presented:
- pain in the right abdomen;
- yellowness of the skin and mucous membranes;
- tuberous compaction in the right hypochondrium;
- loss of appetite;
- significant weight loss;
- nosebleeds.
We suggest you familiarize yourself with Quickly getting rid of a cold under your nose
In this case, there is a significant increase in the volume of the liver and spleen, and the biochemical composition of the blood changes.
Melanoma with metastases is a dangerous disease that is difficult to diagnose at the initial stage of development. The penetration of cancer cells into the liver indicates the progression of the disease. Metastasis occurs by hematogenous route. When blood is filtered by the liver, metastases are retained in the organ. At the same time, a macropreparation is detected in the tissue - areas of accumulation of melanin. Liver damage leads to dysfunction of the organ, which negatively affects the condition of the whole organism, and has the following symptoms:
- presence of seals;
- increase in organ size, tissue tuberosity;
- pain syndrome;
- yellowness of the skin;
- enlarged spleen;
- weight loss;
- loss of appetite;
- frequent nosebleeds;
- violation of the biochemical composition of the blood.
There are disturbances in liver function and bile outflow.
The liver damaged by metastases cannot cope with its functions. The bile duct is compressed until it is completely blocked. Impaired bile flow leads to jaundice. Metastases provoke the establishment of collateral circulation - blood circulation through the lateral vessels. This contributes to the development of palmar erythema, in which the patient's palms turn pink. Bruises appear on the skin due to burst capillaries.
Characteristic
Characteristics of advanced metastatic melanoma include:
- location of distant metastases;
- number and size of tumors;
- an increase in the level of lactate dehydrogenase (LDH) in the blood serum, which usually indicates the spread of the tumor to internal organs.
There are three subclasses of metastatic melanoma. This division is based on the location of metastases and LDH levels:
- M1a: the tumor metastasizes to a distant area of the skin, subcutaneous tissue or distant lymph nodes; LDH is normal.
- M1b: tumor metastasizes to the lungs; LDH is normal.
- M1c: tumor has metastasized to organs other than the lungs, LDH is normal, or there are any distant metastases with elevated LDH levels.
Metastasis occurs when tumors grow beyond their original limits. Against this background, the second stage occurs, the malignant tumor begins to take root in a certain area over time, this process is called metastasis.
With such a disease, it is necessary to understand one important factor: the process quickly metastasizes, which is why organ functioning is disrupted.
Many people are interested in the question, where do metastases occur? Before answering it, you need to know what the penetration routes are.
So, skin metastases in this disease can penetrate through the lymphogenous route. The process of tumor spread occurs due to atypical cells, they pass through the lymphatic ducts. After which the malignant cells penetrate the lymph nodes, and then the skin and internal organs are damaged.
Other neoplasms, directly malignant in nature, can be transmitted hematogenously. In this case, the main route of transmission is the transfer of cells through blood vessels.
When cells spread hematogenously, the following may occur:
- Malignant cells can metastasize to the brain.
- Kidneys or lungs.
- In rare cases, to the adrenal glands.
We suggest you familiarize yourself with Crusts on the head of a 3-year-old child, treatment
Metastases in this disease can be different. For example, if a patient has a neodular form, this means that the malignant cells look like subcutaneous nodes. In the erysipelas form, the patient's skin develops swelling with a purple tint.
In addition, there are two more types of skin metastases. With satellites, multiple rashes are observed, and there is swelling on the skin. The last form is called tromblebitis-like - a painful and fairly dense malignant formation. The skin around the melanoma begins to swell greatly.
What are metastases
Melanoma metastases are a secondary focus of malignancy. The spread of atypical cells occurs in two ways - hematogenous and lymphogenous. In the first way, the spread of metastases occurs through the bloodstream. This type of transmission causes secondary infection of the bones, brain, liver, and lungs. The lymphogenous transmission route spreads metastases with the lymph flow. Spread occurs first to regional lymph nodes, then to distant ones.
Atypical cells settle in lymph nodes, various organs and tissues. Metastasis occurs very quickly in organs that are abundantly supplied with blood - the brain, liver, kidney and lungs.
A characteristic feature of metastasis of pigmented melanoma is the spread of growth islands of malignant tumors on the skin. There are germinations into deeper layers of the skin.
The aggressiveness of the disease is expressed in the fact that spontaneous regressive melanoma occurs - self-destruction of the primary focus, in which the process of metastasis of the lymph nodes is started. This type occurs in 2%.