Skin tuberculosis is a disease whose symptoms are visually visible to others. The causative agent of the disease is Koch's bacillus, a bacterium that is resistant to alcohol, alkalis and acids. This disease ranks 5th in frequency after tuberculosis of other organs. Most often, it is not possible to make an accurate diagnosis immediately; the disease develops in dry and weeping forms, which can be determined by specific symptoms.
It is important for every person to know what the first signs of the disease look like, which will help identify the disease at an early stage. Photos of skin tuberculosis will help you better understand the problem. A timely diagnosis is a chance to fully recover and live a full life.
Causes and routes of infection
Pathology begins to develop after Mycobacterium bacteria or Koch's bacillus enter the body and begin to actively grow, spreading throughout all organs. The microorganism that causes the disease is resistant to the influence of the external environment, high temperatures, and maintains vital activity for a long time in an environment with low temperatures.
Koch's bacillus is not considered a highly contagious infectious agent. Even if a person comes into contact with an infected patient, it is not necessary that he will also become ill. A patient with tuberculosis of the skin or another organ in most cases does not require hospital treatment in the inactive form and is not limited in his movements; he is socially active. In families where there is a patient with tuberculosis, it is recommended not only to monitor his health, but also the hygiene of all members. It is also necessary for everyone to regularly check the body’s reaction to the Mantoux test in order to be able to detect the presence of disease in the body as early as possible.
The main route of infection is airborne droplets through the respiratory system. Less common are household and transplacental methods. The microorganism enters through the respiratory tract, then passes into the bronchial mucosa, alveoli and spreads throughout the body through the bloodstream.
For the human body, Koch's bacillus is a foreign microorganism. Normally, when it gets inside, immune cells attack the pathogen, preventing it from multiplying. The disease can develop in two cases:
- if the immune system is suppressed, there are disturbances in the production of antibodies, a state of immunodeficiency, the body’s defense reactions are weakened by other pathologies;
- if contact with the pathogen is long-term, permanent and the carrier of microbes is at the open stage and does not receive the necessary therapy.
There are a number of factors that provoke a decrease in immunity and contribute to the development of skin tuberculosis:
- smoking is a factor that provokes the development of diseases of the bronchi and lungs, and they, in turn, weaken the human immune system;
- excessive consumption of alcoholic beverages;

- taking narcotic drugs;
- predisposition to respiratory diseases due to structural anomalies, frequent history of illnesses, the presence of chronic inflammatory processes in the respiratory system;
- chronic ailments and inflammatory foci in other organs;
- diseases of the endocrine system;
- diabetes;
- lack of vitamins in the body, poor nutrition;
- neurotic disorders, depression, stress;
- period of bearing a baby;
- unfavorable social and living conditions.
The combination of several factors increases the likelihood of decreased immunity, and therefore infection with the tuberculosis bacillus.
Symptoms
Each type of disease has its own symptoms. But there is a general clinical picture.
- The first signs are the appearance of numerous redness on the skin that hurt or itch.
- Decrease in the level of well-being of the body as a whole.
- A clear decrease in the body's defense response (weakening of the immune system).
- Frequent allergic reactions.
- Positive test for tuberculosis.
We recommend reading an article about methods for diagnosing the disease, namely mantoux and diaskintest.
If you experience at least one of the above symptoms for a long time, consult a doctor immediately. You may be infected, which is dangerous not only for you, but also for all people who come into contact with you.
Classification of skin tuberculosis
There are several forms of the disease. They differ from each other in symptoms and course. The disease has the following forms:
- tuberculous lupus;
- collicative tuberculosis of the skin;
- warty;
- papulonecrotic;
- Erythema induratum of Bazin;
- acute miliary;
- lichenoid;
- miliary-ulcerative.
In addition, experts highlight:
- Primary skin tuberculosis develops immediately after the penetration of pathogenic microorganisms. The secondary form develops after exacerbation of the first lesions.
- Acute miliary disease manifests itself in the form of profuse rashes on the skin with small tubercles, nodules and spots.
- Colliquative is formed in the thickness of the skin and subcutaneous fatty tissue in the form of mobile, round and dense nodes.
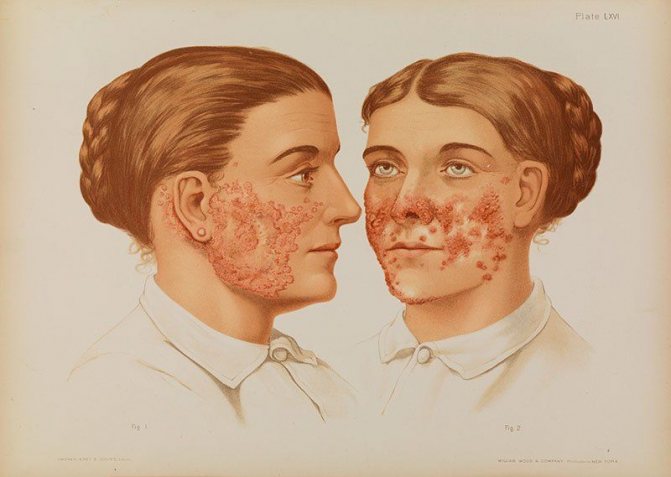
- Tuberculous lupus is considered the most severe form of skin tuberculosis, photos indicate this, in which tubercles appear in the thickness of the skin. They disintegrate and form ulcers and scars.

- Warty is characterized by the formation of bluish-red and gradually growing, merging papules with foci of rough keratinization, and they appear more often on the extensor surfaces of the extremities.
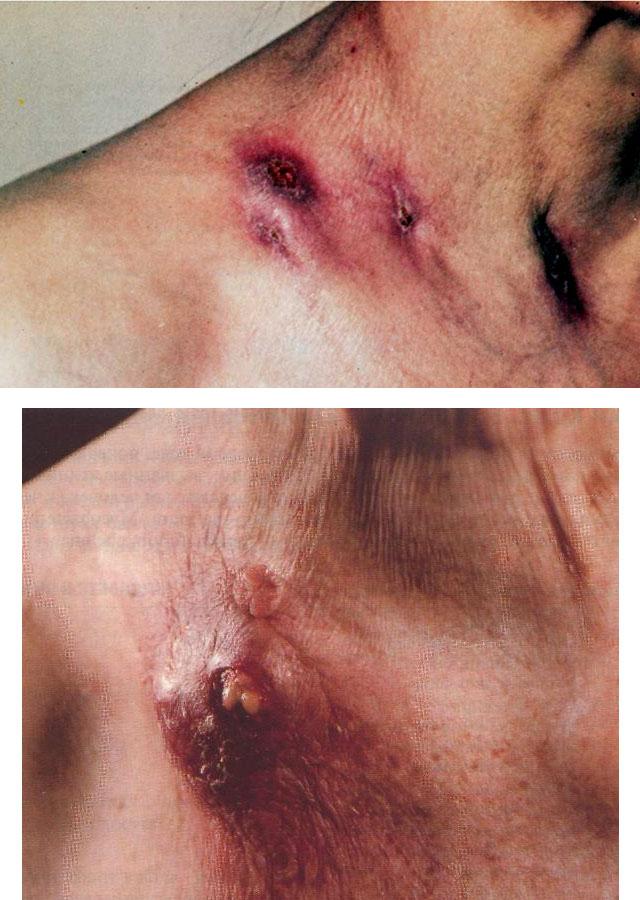
- Scrofuloderma appears as cracks in the skin over suppurating lymph nodes affected by the disease.
- Papulonecrotic manifests itself in the form of the appearance of dense pale red papules on the extensor surface of the legs and arms.
- Indurative manifests itself in the form of dense, round, non-painful subcutaneous nodes with a bluish tint, most often observed on the lower leg.
- Miliary disseminated lupus of the face is characterized by the formation of soft nodules on the face with a reddish-brown tint.
Skin tuberculosis: causes and development
Despite all the types, it has been revealed that skin tuberculosis is one of the rarest forms of the disease . It is believed that the most “favorable” organs for the development of Koch’s bacillus are the lungs, while the skin has a strong protective layer of the epidermis.
The cause of the development of skin tuberculosis is the occurrence of infection against the background of damage to internal organs. In this case, the infection “reaches” the skin through blood and lymph . The disease can also be contracted through external influences. For example, in case of injury to the skin and in direct interaction with the source of infection (a contaminated object, contaminated substances or with a person who already has tuberculosis).
I would like to note that the skin actually has a persistent protective property and the development of cutaneous tuberculosis infection requires the presence of additional factors . These factors include the following:
- unhealthy diet, as well as its uniformity;
- unfavorable environment: poor environmental condition in the area of residence, non-compliance with sanitary standards at home, in living quarters;
- work in hazardous industries: the chemical industry is especially worth highlighting;
- lack of sun: a small amount of sunlight in a person’s life has a negative effect on the skin and the general condition of the body, as there is a “lack of vitamin D”;
- low level of everyday culture in residential premises;
- antisocial lifestyle: neglect of sanitary standards, neglect of contraception.
It can be noted that all factors are certain daily problems associated with limitations in funds, time, fatigue or the person’s reluctance to comply with something. All these aspects, at a certain level of life in a country, can simply disappear or, if implemented properly, turn into a habit of life for every person.
Symptoms
The first signs of skin tuberculosis are difficult to miss. Skin lesions have many types, which differ depending on the stage, shape and type.
- Red lumps appear on the body and face, which can be easily felt - lipomas. If you do not consult a doctor in a timely manner and start therapy, they quickly increase in size.

- The sores may dry out and leave scars in their place. Sometimes they break through and form a weeping ulcer that does not heal. Progression of the disease in severe form can lead to skin cancer and death.
- There is another option for the development of the disease, when small nodules appear, causing discomfort and pain to the patient. Over time, they unite into one large knot with a dense structure.
- If treatment is not started, the skin acquires a bluish tint. The knot becomes soft and breaks out. Purulent discharge appears. After the ulcer heals, a rough scar remains on the skin.
- Warty skin tuberculosis manifests itself as red nodules on the skin. They do not cause pain, but lead to the rapid growth of warts, and after treatment multiple scars appear.
Signs and symptoms of bronchial tuberculosis
Infection by tuberculosis microorganisms has more than one classification. The most common “division” of the types of this disease is the division into focal tuberculosis, or otherwise localized, and widespread tuberculosis, otherwise disseminated. Let's look at each type separately and consider the subspecies. Localized tuberculosis can occur in the following forms:
- Lupus vulgaris (ordinary): one of the most common forms, which most often occurs at a very early age. Skin rashes in this form are localized mainly on the face; in advanced stages, “bumps” may appear in the mouth and on the nasal mucosa. Lupus vulgaris inflammations are located deep under the skin and are yellow-pink in color. However, such spots have clearly visible boundaries. As the disease progresses, these bumps become more and more noticeable, but do not emerge from under the skin.
- Scrofuloderma (colliquative tuberculosis): after lupus vulgaris, this form ranks 2nd in frequency of distribution. This form is characterized by the development of nodules reaching a diameter of 4-5 mm. The nodules are deep, but practically do not cause pain. You can notice them by the blue tint on the skin. As the disease progresses, the nodules can turn into an abscess, which, when opened, may leave an ulcer. As a rule, the reasons for the appearance of this form are called infection from the affected lymph nodes, or from other tissues. This form usually “chooses” the neck or limbs as its location.
- Ulcerative cutaneous tuberculosis: can develop due to infection from various affected tissues and organs. It is characterized by numerous bleeding ulcers on the skin that have yellowish nodules. Such nodules appear, most often, on the mucous membranes and skin surrounding it (genitals, mouth).
- Warty cutaneous tuberculosis: one of the most dangerous and complex types. It is characterized by the appearance of blue-red infiltrates (a kind of compaction, accumulation in a certain place of the body of cellular elements mixed with lymph or blood), which subsequently develop into warts. The causes are external stimuli. This form of skin tuberculosis is called “occupational”, since professions such as veterinarians, pathologists and others are most often at risk of infection. The location is the back of the hand and fingers.
Focal tuberculosis has been dealt with. What about the second type? Disseminated tuberculosis includes the following forms:
- Papulonecrotizing cutaneous tuberculosis: a form that most often appears at a young age. It is characterized by the development of blue-red seals, in the middle of which there are scabs, that is, a crust covering the seal. As a rule, such rashes are located on the buttocks or limbs. It is worth noting that after the scab falls off, a characteristic scar remains on the skin.
- Lichenoid cutaneous tuberculosis: or in other words, the well-known scrofulous lichen. Common rashes that affect the skin of the body.
As you can see, the difference between the two types of skin tuberculosis lies in the scale of the infection. Now we need to figure out the reasons for the appearance.
Despite all the types, it has been revealed that skin tuberculosis is one of the rarest forms of the disease. It is believed that the most “favorable” organs for the development of Koch’s bacillus are the lungs, while the skin has a strong protective layer of the epidermis.
The cause of the development of skin tuberculosis is the occurrence of infection against the background of damage to internal organs. In this case, the infection “reaches” the skin through the blood and lymph. The disease can also be contracted through external influences. For example, in case of injury to the skin and in direct interaction with the source of infection (a contaminated object, contaminated substances or with a person who already has tuberculosis).
I would like to note that the skin does have a persistent protective property and the development of cutaneous tuberculosis infection requires the presence of additional factors. These factors include the following:
- unhealthy diet, as well as its uniformity;
- unfavorable environment: poor environmental condition in the area of residence, non-compliance with sanitary standards at home, in living quarters;
- work in hazardous industries: the chemical industry is especially worth highlighting;
- lack of sun: a small amount of sunlight in a person’s life has a negative effect on the skin and the general condition of the body, as there is a “lack of vitamin D”;
- low level of everyday culture in residential premises;
- antisocial lifestyle: neglect of sanitary standards, neglect of contraception.
It can be seen that all the factors are certain daily problems associated with limitations in funds, time, fatigue or the reluctance of a person to comply with something. All these aspects, at a certain level of life in a country, can simply disappear or, if implemented properly, turn into a habit of life for every person.
Skin tuberculosis, according to the degree of its development, can manifest itself in only two forms: weeping and dry. Consequently, symptoms are divided according to the same criterion.
Dry form
- peculiar blisters appear, after rupture of which the skin can recover;
- After such a rupture, scars appear on the skin, characterized by dry, thin and white skin. The skin is very thin and cannot be softened by any creams. Very often, a new focus of the disease may appear on top of such skin.
Wetting form
- rashes appear that appear as “tubercles”, unlike pimples, have a color closer to brown and do not have a purulent core in their “structure”. Over time, such “tubercles” become covered with scales and crusts, and subsequently grow together into common nodes. They are resistant to antibiotics;
- The skin with the development of “tubercles” is more and more prone to rejection. The “tubercles” are filled with blood and lymph. This mixture, and most often the lymph, is the same infectious substance as the sputum discharge from pulmonary tuberculosis;
- if the “tubercle” is torn off late, an ulcer may remain on the skin.
If skin tuberculosis is detected in a timely manner, treatment will consist of only a few courses of certain medications. It is very important not to neglect this disease, since most often it is skin tuberculosis that affects the upper part of the body and damage to not only the upper tissues, but also the internal ones, namely the brain tissues, will be very dangerous.
Symptoms of skin tuberculosis
A very rare form of primary infection. It is sometimes diagnosed in children or adolescents with an active process in the lymph nodes, lungs, and spine. Active treatment of lupus can also cause the occurrence of scrofulous lichen.
Skin formations consist of group small flat or cone-shaped painless papules. The rashes are symmetrically located on the face, buttocks, or on the mucous membrane of the lips. Externally they resemble eczema. Sometimes they disappear spontaneously, but then reappear.
The patient's condition is generally satisfactory. After treatment of tuberculosis, skin relapses are not observed. In place of the papules, small pigment spots or pinpoint scars remain.
Lichenoid tuberculosis is differentiated from syphilitic lichen, which is accompanied by similar rashes.
It is based on allergic vasculitis as a reaction to the action of toxins of Mycobacterium tuberculosis.
The rashes are paroxysmal in nature. Affects the face, ears, buttocks or extensor surfaces of the limbs. The diameter of the nodules is up to 3 mm. Necrotic crusts are visible in the center, which gradually turn into round ulcers. At the final stage of development they appear as scars with a purple rim.
Often combined with tuberculosis of the lungs and lymph nodes. The disease worsens seasonally. Relapses occur in winter or early spring. Tuberculin tests are positive.
Diagnosis is carried out based on assessment of the type of scars, localization of the rash, and histological studies.
It differs from ordinary tuberculous lupus in the centrally located focus of necrosis in the form of a pustule, and the rapid course of the disease. The lesions do not merge and after healing turn into scars or age spots. Young women suffer from it more often.
Skin tuberculosis, the symptoms of which are very common. Varicose veins, hypothermia of the extremities and standing are factors that provoke the disease. Indurative tuberculosis often accompanies tuberculosis of the lungs, lymph nodes, scrofuloderma, and papulonecrosis infection.
Erythema occurs as a hyperergic reaction to the vital activity of the office with pronounced immunity. It manifests itself as dense, deep and not too painful infiltrates located on the legs, buttocks, and occasionally on the mucous membranes of the nasopharynx. If healed, pigmented scars remain. During the cold season, relapses of the disease are possible.
The greatest difficulty is in differentiating indurative tuberculosis from scrofuloderma and erythema nodosum.
The first symptoms of tuberculosis in adults and children are divided into general and local.
- General symptoms of tuberculosis (intoxication, fever and paraspecific reactions).
- Local symptoms of tuberculosis (depending on the location of the tuberculosis process).
At the initial stages, the clinical symptoms of tuberculosis are extremely scarce, and the signs of tuberculosis in adults and children have weak specificity. The symptoms of tuberculosis at an early stage are similar in nature to the symptoms that occur with a number of infectious diseases. Persons with an open form of the disease (infectious patients) have clinical symptoms in 95% of cases.
- Symptoms of intoxication appear gradually, increase gradually, and are manifested by weakness, sweating, poor appetite, weight loss, and low-grade body temperature.
- Neurovegetative disorders in tuberculosis are manifested by sweating of the palms and feet (distal dyshidrosis), tachycardia, excitability or depression.
- Decreased appetite and subsequent weight loss are associated with constant intoxication of the body.
- Fever in tuberculosis never occurs with a high temperature. Low-grade body temperature is usually noted.
- The first signs of tuberculosis can manifest themselves in the form of paraspecific reactions, which are more often recorded in children. Paraspecific reactions are more often recorded in children (read more below).
Diagnostic methods
Using the Mantoux test, you can assess how sensitive the patient’s body is to tuberculin. To confirm the diagnosis, the doctor may recommend laboratory and instrumental research methods:
- bacteriological analysis of discharge taken from lesions that affected the skin;
- tissue biopsy with further histology;
- Mantoux test;
- studies to determine how much tuberculosis has affected internal organs: bacteriological examination of urine, feces, sputum, X-ray of the lungs, ultrasound of the bladder, kidneys and other organs;
- trial therapy.
Diagnosis of skin tuberculosis will allow not only to make an accurate diagnosis, but also to determine how much the disease has affected the body. The earlier the pathology is detected, the more effective the therapy.
Diagnostics
If you experience any symptoms of cutaneous tuberculosis, you should consult a doctor who will prescribe you the following procedures:
- Mantoux test.
- Chest X-ray.
- Pirquet's test, which detects cutaneous forms of tuberculosis.
It is important to understand that tuberculosis is a complex disease that requires careful diagnosis. Therefore, performing only the Mantoux test in this case is not appropriate. Often, discharge from wounds and ulcers is also taken for analysis.
Treatment
There are several types of treatment for skin tuberculosis. Each of them is recommended for a specific form of the disease. Do not forget that self-medication can only worsen the patient’s condition. If you use traditional medicine methods, then only in combination with traditional ones and after agreement with the doctor.
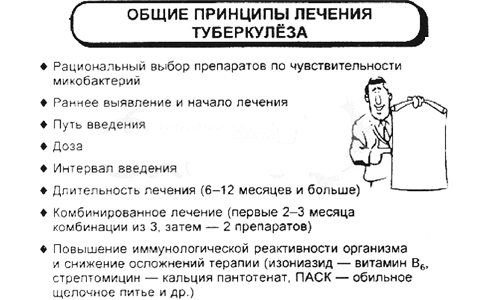
The first and basic rule of treatment is to be under the close supervision of a specialist. General therapy can last from 9 months to one and a half years. Treatment can be divided into several stages:
- Up to 4 medications are prescribed and taken from two to four months.
- Without chemotherapy, treatment will not be effective.
- After a while, the number of drugs is reduced to two, and they are replaced with others. This system does not allow harmful bacteria to develop resistance to the active substances included in the drug.
- An important part of therapy is strengthening the immune system and improving the general condition of the body. To achieve this goal, it is recommended to take vitamin complexes, special diet foods high in protein and vitamin C. The doctor also recommends drinking water properly. To maintain normal water balance in the body.
Often the doctor prescribes electrophoresis to the patient using anti-tuberculosis drugs. This type of treatment gives maximum effect. In rare cases, the doctor may recommend surgery.
Main drugs for treatment:
- specific antibiotics “Rifampicin” + “Isoniazid”; in addition, “Pyrazinamidone” may be prescribed;

It is important to remember that oral medications must be taken daily, without missing a single dose. If you don’t take the medicine just once, it can result in mycobacterial resistance, in which case it will be more difficult to recover.
Traditional methods of treatment
Before using traditional methods of treatment, you need to consult with your doctor, because the etiology of skin tuberculosis is complex and simple lotions may not help. Only a doctor can advise which recipes will be most effective.
Traditional medicine helps strengthen the immune system, saturate the body with protein, vitamins and minerals. Home remedies can reduce the unwanted effects of specific medications. Among the proven and effective remedies are the following recipes:
- You can use herbs such as knotweed, lilac, plantain, coltsfoot, and licorice root internally in the form of infusions;
- decoctions with dry and fresh berries, for example, lingonberries, quinces, strawberries, help strengthen the immune system;
- Infusions with spruce and pine needles will help relieve the inflammatory effect;

- Do not forget about taking aloe juice with the addition of honey, mixed in equal quantities;
- in order to saturate the body with protein, it is better to drink kumiss, if possible;
- To reduce the phenomenon of exudation, you can use ointments for skin tuberculosis with calendula, arnica, wild rosemary, using them twice a day.
In combination with other drugs, you should consume vitamin-containing fruits: apples, red and black currants, rowan, rose hips, viburnum, sea buckthorn, blueberries, etc.
Ancient Eastern medicine recommends the use of many herbal medicines to treat this serious illness.
Diet food
This disease is highly contagious, so it is important to protect others from infection. Is tuberculosis transmitted through skin? Yes, it is transmitted, but only if there are scratches, abrasions and cracks on the skin of a healthy person, so the patient needs to protect those around him and not come into contact with the skin of healthy people.
To recover faster, you need to change your diet from the first days, adding as much protein as possible to your diet. The menu should include: meat, fish, dairy products, milk, whole grain bread.
Be sure to follow the recommendations:
- food should be high in calories, but no overeating;
- be sure to consume fresh lard, butter and vegetable oil, but in reasonable quantities;
- eat as many fresh vegetables and fruits as possible;
- reduce the amount of consumption of baked goods, sugar, sweets;
- drink as many herbal teas, low-sugar compotes, and mineral water as possible.
You should completely avoid drinking alcoholic beverages; they, together with potent drugs, can lead to the death of the patient.
Skin tuberculosis in children
Bacteria that cause a dangerous disease cause trouble for both adults and children. Ulcers, purulent discharge, papules make the child suffer. The use of potent drugs causes undesirable manifestations, allergies, and disturbances in the functioning of internal organs. Therefore, treatment requires strict doctor supervision and constant adjustments. Proper nursing care for skin tuberculosis in children is important. More often, the doctor recommends taking the following medications:
Chemotherapy is carried out for at least 6 months. The dosage and frequency of taking medications are selected individually for each child in accordance with his body weight and the presence of contraindications.

B vitamins are definitely recommended in the form of injections, which prevent nervous system disorders, convulsions, and loss of consciousness. You can protect the liver with the help of hepatoprotectors, and to strengthen the body you will need multivitamins.
Preventive measures
Full compliance with clinical recommendations for skin tuberculosis allows the patient to get rid of this serious illness and continue to live a full life. Especially if the patient follows advice on preventive measures that will protect against re-infection:
- Children must be vaccinated with BCG;
- try to avoid contact with antisocial individuals who can infect a person;
- strengthen the immune system, especially after colds;
- wash your hands well, especially between your fingers;
- less nervous shock;
- Healthy food;
- take vitamins in autumn and spring;
- do not constantly overload the body mentally and physically;
- Avoid contact with an infected person, especially during the period when pathogenic microorganisms are actively being released.
You should not give up when such a serious diagnosis is made. The disease can be cured, but you need to make an effort and follow all the doctor’s recommendations. Skin tuberculosis is a contagious disease, so all family members in contact with the patient must be regularly examined by a doctor, maintain hygiene and not have close contact with the infected person, especially if there are cuts, scratches and other skin damage on the body.
Skin tuberculosis is a complex and serious disease, but with timely treatment there is a chance for a complete recovery.
Even more interesting:
Tongue with HIV infection photo
Yarina or Dimia
In medicine, skin tuberculosis is usually classified as a separate nosological entity that is widespread. The causative agents in this case are tuberculosis microbacteria that penetrate under the skin tissue. The most dangerous varieties are bovine and human tuberculosis (in medicine called Koch's bacillus). You can encounter a similar disease anywhere in the world.
With primary skin tuberculosis, the initial symptoms begin to appear only after a month. A red-brown papule appears at the site of the lesion, has a dense structure and subsequently transforms into a superficial ulcer. This type of disease most often affects young children. After about three weeks, lymphadenitis or lymphangitis begins to appear. By the end of the third month, the affected area of skin heals or, conversely, the process generalizes.
Types
There are two clinical forms of cutaneous tuberculosis: primary and secondary.
- The primary form of the disease appears extremely rarely. This fact is due to the fact that all people are vaccinated against tuberculosis in the first days of life. Primary tuberculosis in most cases occurs in children under fourteen years of age. Red-burgundy inflammations form on the body, in the center of which a whitish tuberculous chancre can be observed. Ulcers do not go away for a long time. After a course of treatment, obvious scars form at the site of inflammation. People with weakened immune systems are characterized by relapses, as a result of which the patient’s body takes on a terrible appearance, spoiled by numerous scars.
- The secondary type of disease occurs in patients who previously suffered from other forms of pathology. Skin tuberculosis is divided into localized and disseminated. Experts conclude that it is precisely these forms of the disease that are appearing more and more often recently. The most common type of disease is dermal tuberculosis, a type of lupus.
There are dry and wet forms.
When dry, the skin continues to carry out regeneration processes, replacing the affected areas with young layers of the epidermis. This form is also characterized by a very dry surface of the infected area, prone to damage.
When it gets wet, erosions form, which do not heal for a long time, and after elimination they form scars.
Tuberculous lupus
Tuberculous lupus or lupoid tuberculosis, as mentioned earlier, is the most common type of disease. This form of the disease takes a long time, is painful and has numerous exacerbations. The infection manifests itself as tuberculous inflammations, lupomas (yellowish tubercles, the size of which does not exceed one centimeter). In the initial stage of the disease, lupomas are located under the fat layer. Over time, they move to the surface of the epidermis. If you put pressure on the lupa, it will burst. This factor will be accompanied by heavy bleeding and severe pain.
- With a positive result of treatment, the inflammation gradually resolves, and in its place a thin layer of very dry skin forms.
- If negative, inflammation appears on the mucous membranes of the eyes, mouth, and nose. At first, lemon-colored plaques form on them, which subsequently lead to tissue necrosis.
There are also scaly and tumor-like types of tuberculous lupus.
Collicative
Colliquatic tuberculosis of the epidermis - mycobacteria enter the skin through the lymph nodes. Thus, small nodules are initially formed under the lymph nodes, which are absolutely painless, but over time they significantly increase in size and begin to cause concern to patients. Later, the nodules open, forming wounds from which pus mixed with blood clots is released. After the pus is released, an ulcerative wound is formed, which, when healed, leaves a scar covered with small papillary growths.
Ulcerative
Men are more prone to this type of disease. Pathogenic mycobacteria come from the sputum or other waste products of a patient infected with tuberculosis. In this case, the skin around the natural openings of the human body is susceptible to pathology. For example, around the mouth or anus.
First, indistinct tubercles form, which gradually fester, forming ulcers. The size of such ulcers can reach up to five centimeters in radius. The course of the disease is extremely difficult. Ulcers take a long time to heal, bleed and fester. All inflamed areas bring severe pain. Frequent relapses are possible.
Lichenoid
This type of disease is also called “scrofulous lichen.” Most often, this disease is observed in children under ten years of age with weakened immunity. Rarely in adults with other forms of tuberculosis. With the described form of the disease, rashes form, which often appear on the limbs and skin of the abdomen.
We recommend reading the article about scrofula on our website.
Warty
Warty skin tuberculosis is observed in people who have been in contact with the carcasses of infected animals. Mycobacteria penetrate the skin with the help of waste products of a dead animal. The disease occurs with numerous complications, and there is a high probability of relapse.
Papulonecrotic
Papulonecrotic tuberculosis of the skin most often occurs in young people. At the same time, small papules are formed on various parts of the body (chest, buttocks, armpits, etc.), the diameter of which can reach up to four centimeters. After healing, they turn into whitish scars.
Indurative
This form of the disease affects patients who suffer from tuberculosis of other internal organs of the body.
Be sure to read the article about extrapulmonary forms of tuberculosis on our portal.
Reasons for appearance
Today there is no clear and specific cause for the appearance of skin tuberculosis, but there are still a number of provoking factors. First, you need to pay attention that healthy skin requires certain conditions for the disease to appear, since it is an unfavorable environment for tuberculosis microbacteria. People with the following problems are at risk:
- Endocrine system dysfunction
- Nervous system disorders
- Disorders of mineral and water metabolism
- Congestion of vascular origin
Social factors also play an important role: living conditions, environmental factors and nutrition. Climatic conditions are no less important - lack of sunlight and dampness can become provoking factors in the development of the disease.
Types of skin tuberculosis
Today, there are two forms of skin tuberculosis - disseminated and focal. Each of them differs in course, causes and methods of treatment.
Collicative tuberculosis of the skin

It is from them that bacteria get under the skin and provoke a secondary disease. With collicvative tuberculosis of the skin (scrofuloderma), symptoms appear on the neck, limbs and jaws. Initially, small and painless nodes appear, which lie in the deep layers of the epidermis and quite quickly increase in size. The skin then takes on a bluish tint and begins to soften right in the center of the spots, forming a continuous bleeding ulcer. In some cases, necrotic tissue departs from the fistula tracts. After the ulcers heal, “ragged” scars remain in their place. Scrofuloderma is observed only in childhood or adolescence. The prognosis for recovery is favorable, provided that the development of the disease has not reached the ulcerative process. Otherwise, the prognosis may be disappointing. For treatment, special anti-tuberculosis drugs and ultraviolet rays are used.
Miliary ulcerative tuberculosis

Appears against the background of existing tuberculosis of the liver, lungs or intestines. With feces, sputum or urine, bacteria penetrate the skin and infect the mucous membranes. The lesions of this form are localized in the sphincter area, nose, and mouth; it appears most often in women. It is characterized by the appearance of small spherical compactions (papules), merging into single lesions and turning into bleeding ulcers. Ulcers are accompanied by severe pain (especially in cases where they are localized in the anus or genital area).
Due to the successful treatment in recent years of all forms of tuberculosis, ulcerative tuberculosis is very rare. The prognosis is favorable, and treatment is based primarily on the treatment of general tuberculosis. X-ray therapy is used, the lesions are treated with a solution of lactic acid. In isolated cases, surgical removal of the main lesion can be used.
Tuberculous lupus

This form of skin tuberculosis is considered the most common. A characteristic feature is a chronic course with slow progression. There are often cases where the disease began in childhood and continued throughout life. In most cases, lesions are localized on the face: nose, cheeks, lips. Lesions of the trunk, limbs and mucous membranes are also found. The first signs of lupoid tuberculosis of the skin are small brown-red rashes. They are soft and smooth to the touch and only later begin to peel off. Lupomas are most often localized in groups at a distance from each other and can merge only with the course of the disease. If you press on the group with a magnifying glass, blood oozes out of them, and the empty holes have a yellowish tint.
In some cases, lupus tuberculosis may look like a tumor, especially when it is located on the tip of the nose or in the ear area. When the lupa disintegrates, large ulcers may form in their place. The disease can develop over many years with barely noticeable progression. Very often, tuberculous lupus can be complicated by skin cancer and erysipelas.
Treatment of this form is very specific and much depends on the clinical picture of the patient, ranging from light therapy to X-ray irradiation. In especially severe cases, surgical removal of the lesions can be used, but most often either liquid nitrogen or a lactic acid solution is used (when the lesions are located on the mucous membranes). The prognosis for tuberculous lupus is in most cases positive and largely depends on the patient’s body’s resistance, timely treatment and diet. But we must not forget that the disease is characterized by slow development and lack of progression, even in the absence of specialized treatment.
Localized forms
Primary cutaneous tuberculosis
It mainly affects unvaccinated children and sometimes adults who have not previously been infected. At the site where mycobacteria enter from the external environment through the wound surface in the skin, after 8-10 days, and in some cases after several weeks, a papule of dense consistency of reddish-brown color appears.
Gradually it transforms into a plaque with painless ulceration. This element is called tuberculous chancre. The lesions are localized, as a rule, on open areas of the body - the face, hands, earlobes (after they are pierced), at the injection site of the tuberculosis vaccine, at the site of a tattoo, sometimes on the feet and in the genital area.
Soon after this (two weeks to 1 month), inflammation of the regional lymphatic vessels (lymphangitis) and lymph nodes (lymphadenitis) develops, with a tendency to decay and ulceration of the latter. Thus, the formation of tuberculous granuloma occurs not only at the site of mycobacterium penetration, but also in the lymph nodes.
Healing of the primary lesion occurs over several months. A scar forms in its place, and an enlarged, dense lymph node remains. In some cases, the process becomes disseminated.
Lupoid tuberculosis of the skin
The second name, tuberculous lupus, is the most common form and accounts for 75%. The disease usually develops in childhood, more often in girls. It can progress over decades and even throughout life, with improvement, mainly in the summer, followed by deterioration.
This form of skin tuberculosis has recently begun to occur in adults, especially among young girls and women. There is a frequent combination of the skin form with damage to internal organs by the tuberculous process. On average, up to 10% of people with lupus tuberculosis suffer from pulmonary, and up to 20% from osteoarticular forms of tuberculosis.
Infection occurs predominantly through the blood and lymphogenous routes; infection by contact is also possible. The lesion manifests itself as a primary element in the form of a tubercle (lupoma), consisting of numerous small nodules. At first, lupoma resembles a red-brown spot with various yellow-brown shades.
Lupoma is a granuloma with a somewhat shiny and subsequently flaky surface. The soft, doughy consistency of the morphological element is due to the destruction of elastic and collagen fibers. When pressing on the tubercle during diascopy (examination through a glass slide), it initially appears transparent (due to the displacement of blood from the capillaries), and then acquires a waxy yellow-brown color (the “apple jelly” symptom).
The tubercles in the center tend to soften and dissolve. Small flat scales appear on them. Subsequently, an atrophically altered scarred area of the skin remains, resembling tissue paper. New tubercles appear in the peripheral zone of the lupoma and in the atrophied area.
Lupoid tuberculosis of the skin
The most typical localization of primary foci of lupoid tuberculosis of the skin is the face, especially in the nose (80%), upper lip, cheeks, and less often - the skin of the limbs and torso.
Clinical types of lupoid lupus:
- flat, the foci of which are located at the same level with the surrounding unaffected skin; the surface of the lesions is not damaged;
- ulcerative, which is accompanied by pronounced, soft at the base, inflammatory infiltration of tissues, subsequent tissue disintegration with the formation of an ulcer with a red, smooth bottom, covered with soft, easily bleeding granulations; the ulcerative edges are undermined and have uneven outlines; the result of healing of the ulcerative surface is the formation of atrophic scars;
- exfoliative, the elements of which are located on the face like a butterfly (the back and sides of the nose, the area of the cheeks near the nose), and therefore there is a similarity with discoid lupus erythematosus; Particularly characteristic of this form is the formation in the area of the lupoma of large, whitish scales tightly adjacent to each other, which sometimes externally resembles psoriasis;
- sarcoid-like, characterized by erythematous foci in the form of tumor-like formations rising above the healthy skin surface;
- Lupus carcinoma is a highly malignant neoplasm that is a complication of lupus tuberculosis.

1. sarcoid-like form 2. flat form

1. sarcoid-like form 2. flat form Exfoliative type of lupoid tuberculosis of the skin
Colliquatic cutaneous tuberculosis or scrofuloderma
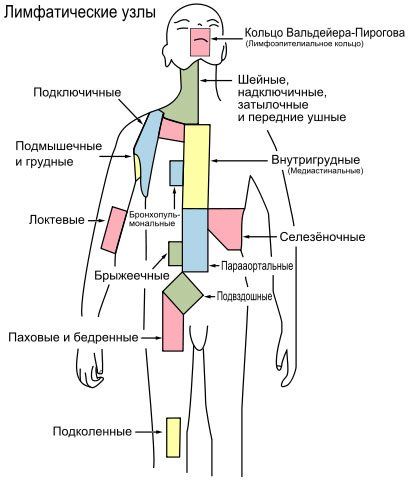
It is in second place in frequency after the previous form. Almost always occurs only in childhood and adolescence. It is a secondary skin lesion. Depending on the route of infection, there are:
- primary scrofuloderma, which occurs as a result of the introduction of the pathogen into the skin by the hematogenous (blood) route and can be localized on any skin areas;
- secondary scrofuloderma, which develops as a result of “contact”, that is, the transfer of the pathogen from the lymph nodes (with lymphadenitis) or, less commonly, from the affected joint or bone to the corresponding skin area.
Since secondary scrofuloderma is more common than primary scrofuloderma, the predominant localization of the disease is the skin areas above the affected lymph nodes - cervical, submandibular, axillary, supra- and subclavian, and elbow.
Collicative tuberculosis of the skin begins with the appearance in the subcutaneous fatty tissue of a dense, mobile, slightly painful or painless node. The node, up to 2–4 cm in size, has a rounded shape and is fused to the unchanged area of tissue located above it.
MORE ABOUT: Salpingitis in women: causes, symptoms, treatment and prevention
Then the hearth gradually melts with the formation of several holes. From them purulent contents with blood and pieces of tissue are released. The resulting ulcers have irregular outlines. Their edges are thin, soft, flabby, undermined, covered with necrotic and purulent discharge, and the bottom of the ulcers is covered with flaccid granulations.
Ulcers heal unevenly and slowly, with the formation of scars in some areas of the lesion and the formation of new ulcers in others. As a result of the uneven formation of scar tissue, the surface of the skin becomes uneven: in some places there are areas of depression, in others there are elevations, and “bridges” and “jumpers” are formed between the scars. In addition, the formation of disfiguring keloid scars is possible.
Collicative tuberculosis of the skin
Warty skin tuberculosis
It most often affects men and children. It develops mainly in persons who, due to the nature of their work, come into contact with people and animals sick with tuberculosis - staff of surgical TB hospitals, pathologists, veterinarians, workers in slaughterhouses, cutting and meat processing shops, etc.
In these cases, the disease occurs as a result of mycobacteria coming into contact with the skin of previously infected people (superinfection). Much less frequently, in persons suffering from various forms of tuberculosis (open forms of tuberculosis of the larynx, lungs, intestines, kidneys), bacterial self-infection (autoinoculation) is also possible.
The localization of the primary tubercle is the dorsum of the hands and fingers, less commonly the anterior surface of the lower third of the legs and the extensor surface of the feet and toes. The tubercle has the shape and size of a large pea, brownish or bluish-red (“cadaveric” tubercle) color.
Slowly expanding at the expense of the peripheral sections, the primary element is transformed into a plaque of dense consistency with massive layers of horny epithelium and warty growths, which resembles a papilloma. After complete development in the lesion, it is possible to determine the peripheral, middle and central zones, presented respectively:
- inflammatory purple-red rim;
- subepidermal microabscesses, hyperkeratotic crusts, cracks and dense grayish warty elevations, upon pressing on which purulent droplets are released from the cracks;
- a smooth atrophic skin area, the bottom of which has an uneven, bumpy surface; it is formed as a result of the resolution of the infiltrate and the development of atrophic processes in its central part.
After resolution of the primary lesion, atrophic scars remain. Positive results of tuberculin reactions occur in 80-96% of patients.
In the area of the peripheral parts of the lesion (usually in children), the formation of new nodules and plaques is possible, gradually merging with each other. These processes are sometimes accompanied by the involvement of lymphatic vessels and regional lymph nodes and a deterioration in the general condition.

Warty skin tuberculosis
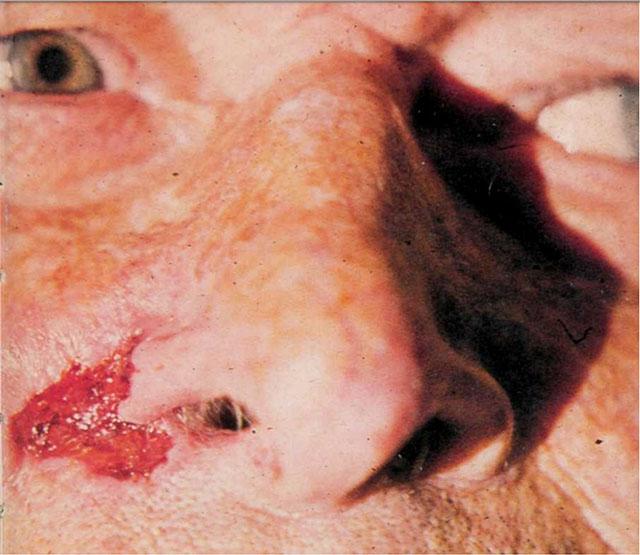
Ulcerative skin tuberculosis, or secondary tuberculous ulcer
It is a rare form of cutaneous tuberculosis. Infection occurs by autoinoculation of microorganisms with sputum, urine or feces in persons suffering from an active form of tuberculosis of internal organs.
Primary morphological elements are inconspicuous spherical yellowish-red nodules or tubercles with a diameter of 1-2 mm, localized in the transition zone (mucous membrane to skin) in the natural area - the nose, mouth, anus and external opening of the urethra.
The nodules very quickly transform into pustules, which merge with each other and open, forming sharply painful small and large (up to 10-15 mm) ulcers that make it difficult to eat or perform physiological functions. The ulcers have a pale red color, soft, somewhat undermined edges and finely scalloped outlines.
Their bottom is covered with flaccid gray, often bleeding granulations and a scanty coating of serous-purulent nature, which contains a large number of pathogens. At the bottom and around the ulcers there are newly formed yellowish nodules with caseous (curdled) degeneration (“Trel grains”). Due to the latter, serpiginizing (serpentine) spread and deepening of the ulcerative surface occurs.
As a result of a sharply expressed immune depression and the absence of a response from the body, the results of tuberculin tests in such patients are negative.
Ulcerative form (secondary tuberculous ulcer)
Symptoms of skin tuberculosis
Tuberculous lupus of the skin

It is the most common form of cutaneous tuberculosis, affecting the epidermis.
It usually occurs in women, children and adolescents. Most often the face is affected, sometimes the buttocks, arms, and legs.
If the disease is not treated promptly, it can lead to the breakdown of the ear cartilage or the cartilage of the bridge of the nose.
In rare cases, it even leads to cancer and even death.
Scrofuloderma, or colliquative tuberculosis of the skin
Women are mainly affected by this form of the disease, most often manifesting itself in the cervical region.
- At first, almost imperceptible, painless nodules appear on the skin; over time, they grow into one dense nodule.
- If the disease is not treated in time, the skin begins to acquire a blue tint, the dense node gradually softens and comes out, and pus is released.
- After this, a deep scar appears at the site of the ulcer.
Papulonecrotic tuberculosis of the skin

It also usually occurs in young women.
- First, small papules that are hard to the touch appear, then a crust appears on their surface.
- If it is removed, small round ulcers form on the surface of the skin.
- Depressed scars remain on the skin.
Erythema induratum of the skin

Most often, the disease affects young women in the lower leg area, where deep and very dense blue-red nodes appear, which sometimes break out (the resulting ulcers in this case take a very long time to heal).
This type of cutaneous tuberculosis has a high tendency to relapse.
Warty skin tuberculosis

Infection usually occurs through injured skin, so it is most common among medical personnel.
The disease occurs on the arms (hands) and feet.
First, red nodules form, which then grow into warty pustules covered with dead skin debris.
Scars remain on the skin in the affected area.
Skin lesions in secondary tuberculosis
Mycobacteria have the potential to penetrate the skin through fresh scratches and cuts. Exposed, unprotected areas of skin are especially vulnerable. The areas of the legs from the knees and below, the feet, and the face usually suffer. The upper extremities are rarely infected.
The resulting skin defect initially heals on its own. But after some, quite a long time, a slight ulceration appears at the site of the cut or small scratch. There is no pain. At the same time, the superficial lymph nodes become softer and increase in circumference.
Diagnostically, if there are noticeable lymph nodes and tuberculosis is suspected, any existing lesions on the skin should be examined. Especially primary scars and scratches. A specific tuberculosis formation is usually small in size, representing a slight thickening, around which there are tiny yellowish spots.
But it may well have the appearance of a smooth scar with uneven, clear edges. If the infection in this area developed for months before the enlargement and softening of the lymph nodes attracted attention.
Small yellow areas around the thickening transform into clear-shaped depressions. This phenomenon is often observed after vaccination: BCG, in fact, provokes a deliberate infection of the skin using weakened strains.
With focal skin tuberculosis, there are two types of abscesses.
- The first is an abscess, which appears just below the surface of the skin as a shallow, soft swelling. It quickly breaks through, forming a small ulcer with a jagged edge. Several abscesses may form simultaneously in different parts of the body.
- The second type occurs at the site of insertion of the needle for intramuscular injection. It is located deeper and mainly in places traditional for injection procedures - on the buttocks, on the outer side of the thigh.
Forms of tuberculous skin diseases are divided into focal (or localized) and disseminated. The following frequently occurring foci are distinguished in the form:
- erythema nodosum,
- tuberculous lupus,
- scrofuloderma,
- verrucous (warty) tuberculosis,
- tuberculides.
The group of disseminated species includes miliary tuberculosis, papulonecrotic tuberculosis, and the so-called scrofulous lichen.
It is observed in individuals with immune resistance to tuberculosis disease. Usually it affects contingents whose occupations come into contact with pathogenic material or with sick people with active forms. These are medical personnel, doctors, veterinarians, pathologists, butchers, etc. The pathology in this case is caused by superinfection. In children, it can occur as a result of skin trauma.
Wart formations appear on areas unprotected by clothing - the back of the hands and fingers. The lymph nodes are not significantly enlarged. First, a dense blue-red tubercle up to 1 cm appears, similar to a corpse. Then it grows, turning into a flat plaque with keratinized layers and warty growths.
The formed focus of verrucous tuberculosis has areas rising one above the other: a characteristic colored border, warty cracks, crusts and an atrophic area with a tuberous bottom in the center.
Warty growths are characterized by subcutaneous abscesses. When pressure is applied to them, specific purulent discharge appears. Fresh plaques form around the main focus, tending to merge.
The test for tuberculin is positive in almost one hundred percent of cases. The clinical condition of adult patients is usually good. After treatment, scar modifications of the skin remain at the site of infection; new warts do not form in these areas. In children, the condition may be impaired due to lymphangitis and lymphadenitis. The formation of new tubercles along the perimeter of the old lesion is possible.
The course of the disease is long-term and chronic. But the prognosis for recovery is favorable. In addition to standard conservative treatment, radiation therapy and high-frequency currents are used to stop pathological tissue proliferation (diathermocoagulation).
To prevent the development of such a disease, it is necessary to observe basic rules of personal hygiene and avoid contact with carriers of tuberculosis. Nutrition is very important. The daily diet should be balanced. It is necessary to regularly consume fish, dairy products, honey, fresh vegetables and fruits.
You should undergo a full medical examination every year. As for children, there must be constant doctoral supervision in kindergartens and schools. Parents should monitor the cleanliness of their children's skin and, if tuberculosis is suspected, consult a doctor immediately.
Public awareness and promotion of knowledge about tuberculosis play an important role in the fight against tuberculosis.